|
Onions are an overlooked vegetable. Whether they’re being sautéed for a soup, sliced for a burger, or pickled for a salad, onions rarely steal the show of a meal, although they often inspire a sob story.
Onions are most known for their pungent flavor, not necessarily their nutritional value. Their white flesh (even in red onions) isn’t always perceived as being as nutritious as vibrantly colored vegetables like kale, broccoli, or beets. But that’s no reason to snub onions. Although some onion varieties are lacking in color, onions in general are one of the highest natural sources of a powerful flavonoid: quercetin.1 What is quercetin? Quercetin is a flavonoid, which is a chemical compound found in plants. In addition to onions, quercetin is also found in many other fruits and vegetables like capers, asparagus, and apples, as well as tea and red wine.1 A single serving of onions is considered to be one medium onion, which contains around 52 milligrams (mg) of quercetin.2 But most people tend to not eat a whole onion in one sitting (unless they really like onions), so you’re probably not getting quite that much quercetin when you eat onions. Even with all these natural sources of quercetin, it’s estimated that most people following a typical Western diet (think higher in simple sugars and animal products and lower in produce) only get 0 to 30 mg a day.1 That’s not a lot, considering research shows that some of quercetin’s health benefits are reached at supplemental intake levels, not from a food source, of 500 to 1,000 mg per day.3 Quercetin and health Quercetin is one of the most studied dietary flavonoids and is associated with multiple health benefits. Two of this compound’s most notable benefits are supporting heart health and protecting against oxidative stress. Heart health: Quercetin plays a positive role in supporting healthy blood pressure and endothelial health.4 The endothelium is the thin layer of cells lining the body’s blood vessels and heart. It is considered an active organ in the body as it helps control when blood vessels relax or constrict.5 Protection against oxidative stress: Everyone undergoes oxidative stress, which is caused when there is an imbalance of harmful free radicals, which damage cells and tissues. This process happens inside the body, so although you may not feel immediate effects from oxidative stress, it can affect both health and the immune system over time. Antioxidants can help quell some of that stress. And since quercetin acts as a free radical scavenger and supports antioxidant processes, it’s especially good at this.3 Getting the most quercetin out of onions Because these health benefits are mainly seen at higher levels of quercetin intake, it’s important to maximize what you can from the diet. Here’s how you can get the most quercetin when eating onions.
Onions are a rich, natural source of the flavonoid quercetin. High intakes of quercetin are associated with cardiovascular benefits and oxidative stress protection. However, quercetin is not a “magic bullet” to health. Instead, focus on eating a plant-forward diet with lots of produce and know that onions, albeit smelly, are a healthful choice. References:
0 Comments
Feeling bloated during pregnancy? While inconvenient and uncomfortable, most forms of swelling—also known as edema—are perfectly normal for expecting mothers.1
Why does swelling occur during pregnancy? Among the many changes the body goes through during pregnancy is its production and retention of water, blood, plasma, and other fluids to support the needs of the developing fetus.2,3 The swelling supports the mother’s development, as well. Not only does the extra fluid help her body expand to accommodate the baby, it also helps with her body’s necessary changes to prepare for the actual delivery process.1 Most mothers-to-be have swelling in their extremities, as well as in the face.1 Swelling tends to peak during the third trimester, often becoming more noticeable at the end of the day, when extra fluids, blood volume, and the growing baby can affect blood flow in the ankles and feet.4 What other factors affect swelling during pregnancy? A number of factors in addition to the changes taking place in your body can affect swelling.1 These factors include: 1
While mild swelling is acceptable during pregnancy, a very sudden bout of edema could actually be more concerning.1 Contact your doctor immediately if the swelling is uneven and painful, if it comes on suddenly, or if it is accompanied by shortness of breath or chest pain.5 How can you address swelling during pregnancy? There are a number of strategies you can leverage to reduce swelling during pregnancy.1, 5-7 You might make a point of:
Dietary tips to reduce swellingThere are also a number of dietary tips that can help to reduce swelling during pregnancy. These include:
Additional therapies to tryIn addition, pregnant women might try to lessen swelling and related symptoms by engaging in therapies like:
You can either ask your partner to gently massage your feet and legs with the essential oil or soak your feet in a bowl of warm water mixed with essential oil.6
While research offers mixed results on the link between reflexology and swelling, some experts believe the practice can minimize the discomfort associated with swelling.8 Interested in scheduling a reflexology session? Be sure to select a registered specialist who has extensive experience treating pregnant women. Ultimately, there are a number of best practices for reducing swelling during pregnancy.1,5-8 If you still experience swelling after delivering your baby, simply be patient and allow your body time to heal.5 You may still be going through hormonal changes that exacerbate the swelling.5 And of course, feel free to reach out to your healthcare provider at any time if you have questions. References: 1. American Pregnancy Association Staff. Swelling During Pregnancy. https://americanpregnancy.org/pregnancy-health/swelling-during-pregnancy/. American Pregnancy Association. Accessed August 13, 2019. 2. Widen et al. Body composition changes in pregnancy: measurement, predictors and outcomes. Eur J Clin Nutr. 2014;68(6):643-652. 3. Vricella LK. Emerging understanding and measurement of plasma volume expansion in pregnancy. 2017;106(Suppl 6):1620S-1625S. 4. Tanveer F et al. Frequency of lower extremity edema during 3rd trimester of pregnancy. SAJMS. 2015;1:41-43. 5. UnityPoint Health Staff. Things That Make You Swell When You’re Pregnant.https://www.unitypoint.org/livewell/article.aspx?id=e668bf44-c376-459e-b263-41f48810373a. LiveWell with UnityPoint Health. Accessed August 13, 2019. 6. Baby Centre Medical Advisory Board Staff. Swelling (natural remedies).https://www.babycentre.co.uk/a549316/swelling-natural-remedies. BabyCentre UK. Accessed August 13, 2019. 7. Tobah YB. What causes ankle swelling during pregnancy—and what can I do about it?https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-answers/swelling-during-pregnancy/faq-20058467/. Mayo Clinic. Accessed August 13, 2019. 8. Embong NH et al. Revisiting reflexology: Concept, evidence, current practice, and practitioner training. J Tradit Complement Med. 2015;5(4):197–206. By Cassie I. Story, RDN
Have you begun to feel the cool crisp air on your skin? Perhaps you have noticed the leaves turning from emerald green to pale orange. On the other hand, maybe you live in a mild-tempered climate that stays the same year round, with the ocean waves leaving little hint for seasonal changes—but traces of fall and pumpkin spice everything have made their way to stores near you. While planting a garden may seem so last season, it is not too late to enjoy homegrown (literally) produce that will be ready just in time for a fall harvest. Not only can starting a garden bring you a literal bounty of food, research has shown that it offers a host of health benefits as well. Studies have shown that gardening may improve an individual’s life satisfaction, vitality, and psychological wellbeing; supports cognitive function; and can increase a sense of community and togetherness.1-2 A 2017 meta-analysis suggests that gardening activities have various significant positive effects on health including reductions in stress, mood disturbance, and body mass index.3 The analysis also notes several enhancements in quality of life measures like a sense of community, increased physical activity levels, and improved cognitive function.3 Several possible mechanisms were suggested through which gardening may promote health, although it may be difficult to unravel the causal relationships between gardening and health.3 The pathways that the authors suggest for the health impact of gardening may be the benefits of direct experience with nature, the uptick in physical energy expenditure, the opportunity to engage with members in the community via community gardens or produce sharing, and lastly by increasing fruit, vegetable, and herb intake.3 Gardening has been shown to improve quality of life and health across the lifecycle. Intervention studies on children and college-aged students have shown an increase in daily fruit and vegetable consumption when participants recently participated in gardening activities.4 Observational studies on aging populations have found that maintaining a home garden is associated with restorative and physical benefits, increased positive feelings, and a sense of pride, creativity, and achievement.5 If you are ready to dig in, there is no need for space or climate to be an issue. If you are new to getting your hands dirty, a container garden can be an easy and less intimidating way to start! Here is your step-by-step guide to getting your container garden growing. 1. Choose your container(s). Start with a large container or pot that is at least 15 inches deep and wide. If you are a beginner gardener, bigger is better because you can hold more soil and lock moisture in longer. Large flowerpots, barrels, baskets, planters, or any other large container will work—get creative and choose something that speaks to you. The container or pot must drain well. Ensure there is at least one hole in the bottom for water to flow out. If your container does not have drainage holes, use a drill to create 4-6 holes throughout the bottom for even clearance. Choose one vegetable or herb for each container, especially if this is your first time gardening. It is important not to overcrowd the pots. 2. Place container in an appropriate area. Choose an area that receives about six hours of sunlight a day. You may need to move the container throughout the fall depending on the weather (frost, wind, etc.). If you live in cooler areas of the country, you may need to cover your produce with a light cloth overnight to prevent frostbite. If you have room, try placing it on a small cart or wooden box so that you can easily move it to a more desirable area as the weather and sun pattern change. 3. Plant! Purchase high-quality, organic potting mix designed to retain moisture well, along with quality plant starts or seed packets from your local garden store. Fill the base of the container with an inch or two of small rocks or pebbles to help drainage and to prevent mold or mildew. Add soil to the container, leaving about two inches of space from the top. Thoroughly water the soil and let drain for a few hours before planting the seeds or starter plant. For seeds, plant according to package directions. For starter plants, dig a hole deep enough for the soil to reach the same level they were growing in the container in which they came. 4. Water your new plants. Maintain moisture levels. The soil should feel moist about one to two inches below the surface. Depending on the climate you live in, you will likely need to water your plants multiple times per week. In the intense Arizona sun, where temperatures can continue well over 100 degrees Fahrenheit through November, I oftentimes find myself watering twice a day to maintain optimal moisture. Watering in the morning is preferred to the evening, because it helps the plants stay hydrated during the heat of the day. Late summer, early fall vegetables What to plant from a plant start (with fruit already on the vine):
Ten seed vegetables to plant in late summer for a fall harvestPlant the seeds half an inch to a full inch deep and about one inch apart in each row: Beets, broccoli, cabbage, carrots, cauliflower, peas, radishes, sage, snap peas, squash Whether you are a novice or seasoned gardener, planting a container garden can be an easy and rewarding experience. I hope this article inspires you to get your hands dirty and play with your food! References: 1. Gonzalez MT et al. J. Adv. Nurs. 2010;66:2002-2013. 2. Wood CJ. J. Public Health. 2016;38:e336-e344. 3. Soga M et al. Preventive Medicine Reports. 2017;5:92-99. 4. Loso J. J Acad Nutr Diet. 2018;118(2):275-283. 5. Scott TL et al. SAGE Open Med. 2020;8:2050312120901732. By Michael Stanclift, ND
Coenzyme Q10 (CoQ10) may sound like a code name for an eccentric secret agent, but this versatile compound’s aliases indicate how common it is in the natural world. CoQ10 also goes by the names ubiquinol or ubiquinone.1 It’s a fat-soluble antioxidant that affects all cells in our bodies and is especially important for the powerhouses of our cells, our mitochondria.1 Most of the benefits from CoQ10 come from its ability to protect cells and their components from oxidative stress and its ability to produce energy in our mitochondria.1 So who might benefit from CoQ10? Anyone looking to enhance the health of these bodily systems: Musculoskeletal health: Our muscles have a ton of mitochondria in them, and in turn they really like CoQ10.2 If our muscles don’t have enough CoQ10, they can become tender, and we might experience more fatigue.1 In some cases, taking CoQ10 supplementally can help with discomfort, tenderness, and fatigue.1 Cardiovascular health: On a related note, our hearts are also loaded with mitochondria and are essentially muscles that never rest.3 CoQ10 can help improve contractility of our heart, prevent the oxidation of LDL (bad) cholesterol, maintain healthy blood pressure, and support the delicate endothelial layer that lines our blood vessels.1 Some medicines, like HMG-CoA reductase inhibitors, commonly known as “statins,” inadvertently blunt our ability to make our own CoQ10, so can reduce what we have available.1 In situations such as this, supplementing CoQ10 may help.1 Glucose control: Research shows CoQ10 supplementation can support long-term healthy blood sugar levels.1 Neurological protection: Our highly active brains don’t make up a big percentage of our weight, but they certainly consume a lot of our energy in calories.4 All that energy consumption has the potential to result in oxidative stress, requiring a steady supply of antioxidants.1 Also, remember that our brains have a lot of fat in them, and as CoQ10 is the only internally produced fat-soluble antioxidant, it is precious in our cranium-encased think organs.1 Research shows that CoQ10 levels in our brains are important, and having an adequate amount can be protective.1 Sperm health: Sperm have the important job of delivering half a set of genes to an egg, and the “delivery” part of that job relies on, you guessed it, mitochondria.5 You’ve probably seen a microscope view of sperm, those tadpole-shaped cells with a head (housing DNA) and a tail. Between the head and tail are a collection of tightly wound mitochondria, which power and propel the whip-like tail and cause the sperm to swim.5 Therefore, CoQ10 plays an important role in the health of sperm. Because CoQ10 is pivotal in our abilities to produce energy in our cells and protect them from potential damage from this energy production, it’s needed in all cells. CoQ10’s importance becomes most apparent in our most metabolically active tissues such as our muscles, hearts, and brains. If you’re looking to enhance the health of these organs, then ask your healthcare provider if supplementing CoQ10 is a good idea for you. References:
By Michael Stanclift, ND You’re feeling that rush as you catch your stride on your morning run. The air is perfect. Suddenly a cramp or muscle ache stops you dead in your tracks. You try to shake it off, but it just grabs more. Ah! We still don’t completely understand why muscles tighten up involuntarily. Exercise, pregnancy, electrolyte imbalances, nerve compression, and diminished blood supply to the muscle all may contribute.1,2 So what can we do to combat these harmless but pesky discomforts? In this article we’ll look at what the research says. Surprisingly, some popular natural remedies don’t shine through in the current medical evidence. What might not help with cramping Magnesium and Epsom salts: A Cochrane Review found that oral magnesium wasn’t likely to help with muscle cramps in older people, and the findings were inconsistent in pregnant women.3 A recent randomized, placebo-controlled trial in pregnant women found no difference in leg cramps with magnesium compared to placebo.4 Epsom salt (magnesium sulfate) baths have long been a go-to for muscle relaxation, and “float” centers with sensory deprivation tanks full of the magnesium-rich water have popped up as an urban refuge from the constant stimulation of modern life. A study in nonathletic healthy men found a one-hour float (in magnesium sulfate) after exercise reduced pain perception compared to one hour of passive recovery.5 However, these findings are tough to attribute to magnesium, as the study’s control didn’t match other potentially therapeutic factors, such as body positioning and sensory deprivation.5 So a relaxing bath may help with cramping and muscles, but it’s unclear if adding Epsom salt makes a significant difference. Active cool-down and static stretching: Many believe after exercising intensely a period of low-to-moderate intensity will prevent muscle soreness and injuries, but this doesn’t appear to be true.6 A 2018 review found evidence on active cool-downs shows it doesn’t significantly reduce soreness, stiffness, or range of motion and may inhibit muscular glycogen resynthesis (energy storage).6 This same review found that static stretching before or after exercise didn’t reduce muscle soreness.6 What might help with muscle cramping: Foam rolling: This surprisingly simple tool can be valuable if you suffer from muscle soreness and cramps. Using a foam roller after exercise can reduce muscle soreness and improve athletic performance the following day.6 Physical therapists from Harvard agree that 30-120 seconds per area can be helpful in relieving sore muscles and preventing cramps.7 Muscle soreness: Tart cherry or pomegranate juice: A small randomized, double-blind, placebo-controlled trial found 355 ml (~12 oz.) of tart cherry juice drunk twice a day for a week before a 26 km (16-mile) run reduced the amount of pain reported from participants.8 A research review found similar effects from drinking tart cherry juice twice a day, and one study found pomegranate juice reduced soreness.9 But the research on these two drinks in relation to muscle soreness has shown mixed results.9 A recent study compared tart cherry, pomegranate, and placebo drinks to analyze the impact on muscle soreness in nonresistance trained men.10 In this study, the researchers were surprised to find that neither of the fruit drinks appeared to help with muscle soreness when compared to placebo.10 Ginger: In a small double-blind, randomized, placebo-controlled trial in experienced runners, 5 days of powdered ginger supplementation (1.4 g/day) moderately reduced muscle soreness from a run (on day 3) during the supplement period.11 A review of randomized clinical trials found that consuming up to 4 g of ginger postintense exercise can reduce muscle soreness and improve muscle recovery.12 Lower single dosages of 2 g ginger did not help with muscle soreness when compared to placebo.12 This suggests it may take multiple days or higher doses to get the effect. Curcumin: It’s no surprise that curcumin, a bright orange compound from the spice turmeric is making news again. A research review found curcumin in a wide range of doses (150 mg-5,000 mg) can reduce muscle soreness after exercise.13 Curcumin can work when used on an “as needed” basis, with even a single dose (150-200 mg) showing effectiveness for muscle soreness following exercise.13 Interestingly, in this review they found small doses (90 mg twice a day) of curcumin taken for 7 days before exercise had no effect on postexercise soreness, while the same dosage taken after exercise for 4 days was effective.13 Other studies in the review at similar doses did not find curcumin improved muscle soreness compared to placebo, so differences in the trial participants and types of exercise may influence the effects.13 Conclusion:Cramping and muscle soreness can ruin a good exercise session, but they don’t have to. When it comes to combatting these annoying aches, you have numerous options—but beware that some popular natural treatments might be more hype than help.
References: 1. Young G. Leg cramps. BMJ Clin Evid. 2015;2015:1113. 2. Mayo Clinic Staff. Muscle cramps. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/muscle-cramp/symptoms-causes/syc-20350820#:~:text=Overuse%20of%20a%20muscle%2C%20dehydration,Inadequate%20blood%20supply. Accessed February 11, 2021. 3. Garrison SR et al. Magnesium for skeletal muscle cramps. Cochrane Database Syst Rev. 2012;2012(9):CD009402. 4. Araújo CAL et al. Oral magnesium supplementation for leg cramps in pregnancy-An observational controlled trial. PLoS One. 2020;15(1):e0227497. 5. Morgan PM et al. The acute effects of flotation restricted environmental stimulation technique on recovery from maximal eccentric exercise. J Strength Cond Res. 2013;27(12):3467-3474. 6. Van Hooren B et al. Do we need a cool-down after exercise? A narrative review of the psychophysiological effects and the effects on performance, injuries and the long-term adaptive response. Sports Med. 2018;48(7):1575-1595. 7. Harvard Health Staff. Roll away muscle pain. Harvard Health Publishing. https://www.health.harvard.edu/staying-healthy/roll-away-muscle-pain#:~:text=Foam%20rollers%20are%20easy%2Dto,from%20exercise%2C%20and%20reduce%20injury.&text=As%20you%20age%2C%20occasional%20muscle,lightweight%20cylinder%20of%20compressed%20foam. Accessed February 11, 2021. 8. Kuehl KS et al. Efficacy of tart cherry juice in reducing muscle pain during running: a randomized controlled trial. J Int Soc Sports Nutr. 2010;7:17. 9. Bowtell J et al. Fruit-derived polyphenol supplementation for athlete recovery and performance. Sports Med. 2019;49(Suppl 1):3-23. 10. Lamb KL et al. No effect of tart cherry juice or pomegranate juice on recovery from exercise-induced muscle damage in non-resistance trained men. Nutrients. 2019;11(7):1593. 11. Wilson PB. A randomized double-blind trial of ginger root for reducing muscle soreness and improving physical performance recovery among experienced recreational distance runners. J Diet Suppl. 2020;17(2):121-132. 12. Rondanelli M et al. Clinical trials on pain lowering effect of ginger: A narrative review. Phytother Res. 2020;34(11):2843-2856. 13. Yoon WY et al. Curcumin supplementation and delayed onset muscle soreness (DOMS): effects, mechanisms, and practical considerations. Phys Act Nutr. 2020;24(3):39-43. Difference between vasomotor and other symptoms of menopause
By Monazza Ahmad, B.Pharm, MSc Menopause is undeniably the most confusing phase of a woman’s life. The irregular menstrual cycle and unpredictable biological changes and emotional state can negatively affect her social, work, and daily life. Seeking help for these symptoms could feel awkward since many times women don’t know how to communicate these concerns and whether it would be empathetically understood or not. At times, the complex medical terms associated with menopause can make it tough to follow the course of treatment plan. Let’s discuss the major signs and symptoms of menopause and the terminologies associated with it that may help you understand your situation as well as convey your concerns to your provider. What are vasomotor symptoms (VMS)? The word “vaso” is originated from the Latin1 meaning vessel, and “motor” relates to movement. So vasomotor symptoms are the movement of blood vessels characterized by their constriction and dilation that causes temporary irregular blood pressure that in turn alters the body temperature, making us feel hot or sweat.2 This temperature alteration results in hot flashes and night sweats that are the most common indication of perimenopause and menopause.3,4 Other chronic and progressive symptoms are characterized by vaginal dryness, painful intercourse, and reduced lubrication. It is seen in both premenopausal and postmenopausal phases.5 Why do I feel like I’m the only one suffering from these symptoms? During menopausal transition, the vasomotor symptoms impact about 80% of the women in the US and differ widely from region to region.6,7 Even though a variety of symptoms is common during menopause, some are not much reported due to their mild and nonspecific nature. Up to 84% of postmenopausal women tend to just deal with the menopausal discomfort rather than seeking medical attention.5,8 How long do these symptoms last? Don’t worry if you have been experiencing vasomotor symptoms for more than a few years. For many women, it can last over a decade or two, with 4-20 hot flashes daily being common during menopause.9 A new long-term study of women from various races and ethnicities suggests that hot flashes and night sweats can take up to 11 years to resolve for some women. Interestingly, the study further discovered that hot flashes lasted longer, for 9-10 years, if started before the menstrual period ended, while their duration was much shorter, with 3.5 years if women had their first hot flash after the periods ended.10 Some menopausal symptoms can get worse with age as opposed to the other menopausal symptoms that improve with time. How do these symptoms impact women’s quality of life? Hot flashes, night sweats, vaginal dryness, low libido, sleeplessness, and menopausal anxiety all add to the decline in quality of life. The sudden outburst of sweat with hot flashes can be daunting when it occurs in a gathering, making women nervous. Vaginal dryness and decreased interest in sexual activities go hand in hand, impacting intimate relationships. All of these stressful changes in daily routine are enough to make any woman anxious.5 Some of the other concerns include brain fog, urinary incontinence, weight gain, hair loss, bone loss, and heart health, to name a few.11 Therefore, women are highly encouraged to not ignore menopausal discomfort and instead have informed discussions with their healthcare providers to find safe solutions for their health needs.12 What are my relief options? There are several options to reduce the impact of these menopausal symptoms and claim your lifestyle back. The solutions include prescription medications, well-studied supplements, lifestyle changes, and nutrition. Since the trial and error of wrong choices can become painful and lengthy during menopause, it is important to discuss the best option with your provider at the right time. Hormone replacement therapy (HRT): This is the most common prescription option for hot flashes, but it is not usually the first choice. The common forms are tablets, gels, skin patches, injections, and vaginal inserts. HRT is generally best-suited for healthy women and those that are in the early phase of menopause. It is not recommended to start HRT after the age of 60. However, there are some side effects associated with HRT, and it is generally considered unsafe for people with a history of heart conditions, deep vein thrombosis, cancer, and smoking.12 Rheum rhaponticum (ERr 731®): This nonhormonal solution is the top recommended natural ingredient by OBGYNs. It has shown to improve 12 of the main menopausal symptoms by 83%. In addition to hot flashes and night sweats, it also improves sleep disturbances, mood swings, sexual discomfort, anxiety, vaginal dryness, and muscle and joint health, to name a few.13 Lifestyle: Daily physical activity is important for menopausal symptom relief. Weight management, stress relief, increased metabolism, and improved overall quality of life as a result of active movement are all related to better management of menopause.14 Eating habits, consuming a healthy diet, practicing relaxation or meditation, drinking enough water, getting quality sleep, and avoiding smoking and alcohol all help with relieving the menopausal discomfort.15 Nutrition: Taking necessary supplements or eating food rich in vitamin D, E, B6, folic acid, and omegas help reduce intensity of menopausal symptoms.16 Now that you have learned more about menopausal symptoms and their treatment options, you may want to discuss these concerns with your healthcare provider. In our next post, we will go over a few tips on how a patient and their healthcare provider can effectively communicate these menopausal challenges with each other to come up with the best treatment plan. References:
By Monazza Ahmad, B.Pharm, MSc To ensure best health outcomes in a healthcare setting, it is important to establish open, effective, and respectful communication between a patient and a healthcare practitioner. As a patient, it is not only your right but in your best interest to ask your doctor for clarification or further explanation on your health condition and treatment plan. As a healthcare provider, it is your responsibility to provide a safe and comfortable environment for your patients to openly discuss their health concerns and make sure your diagnosis and treatment plan is well understood. That said, menopause can trigger many complex and confusing symptoms that can be uncomfortable to talk about, which can make managing the symptoms difficult. Here are some tips for both patients and practitioners to start the conversation around menopause and its symptoms that we discussed in our previous post, Menopausal Symptoms. When should I talk to my doctor about menopause?1 First of all, don’t feel awkward. Menopause is a natural phase of life, and your doctor is likely familiar with all possible symptoms. Describe your condition and symptoms in detail and explain how they are affecting your lifestyle and relationships. The provider needs to rule out any other underlying conditions before determining it is menopause. Reach out to your doctor if:
Don’t forget to tell your doctor if you have any allergies or other health conditions. Also mention any medications or supplements you’re already taking for menopause symptoms or other conditions. What shall I ask my doctor? Medical appointments can be stressful, and we often feel rushed. When you have a delicate issue to bring up, being prepared can help. Here are some of the questions you can ask your practitioner:
How can healthcare providers ensure the right care during menopause? Often, the reluctance from healthcare professionals to address these female issues can also cause lack of awareness. It is the healthcare provider’s obligation to make sure patients feel comfortable in discussing their menopausal concerns and understand the treatment plan.2 According to a survey by NIH, patients are likely to discuss menopause transition with providers who don’t make them feel rushed, are good listeners, and have expertise in this area of women’s health. Here are some ways to help your patients receive the best care:
What to ask your patients:3
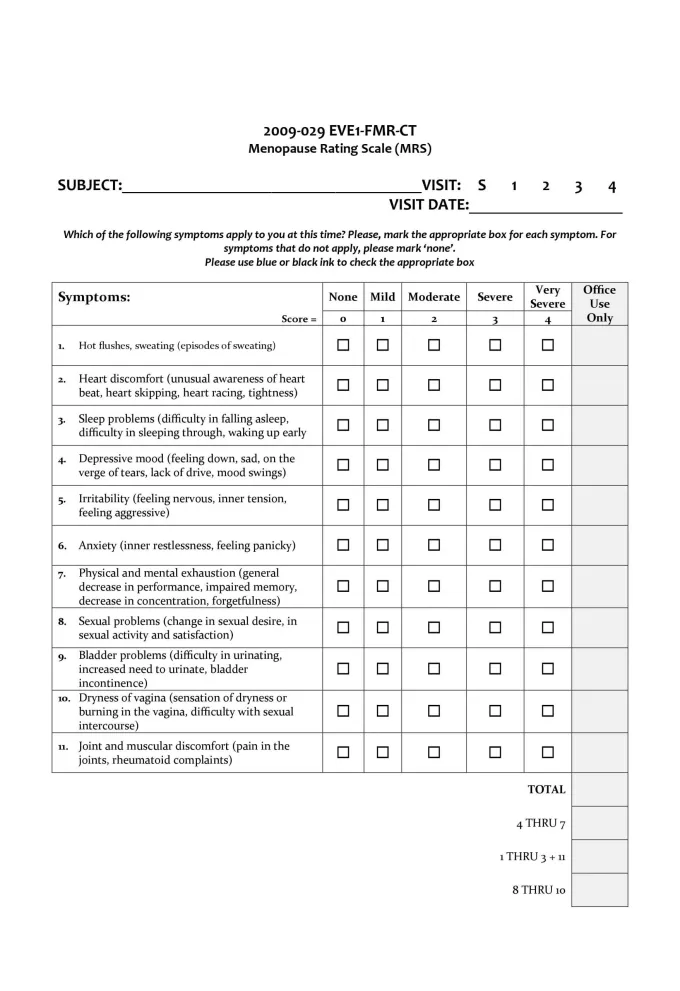
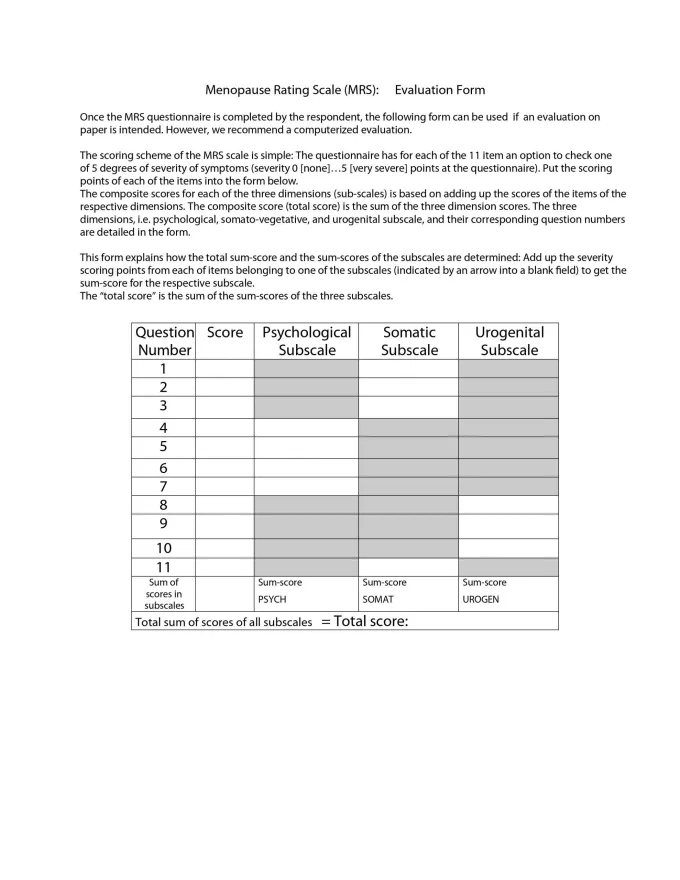
Menopause symptoms evaluation form and rating scale (click to enlarge)Menopause is a natural phase in a woman’s life, and its challenges need to be accepted and understood at work, at home, and on a social as well as a societal level. Unless these concerns are progressively communicated in a healthcare setting, it will be tough for us to understand the impact of this condition on a woman’s life.
References:
By Whitney Crouch, RDN, CLT
While running around being a “stay-at-home” mom, a “9-5” mom, or somewhere in between, it can be easy for mothers to forget about taking care of themselves. Breastfeeding mothers may face an added layer of stress when trying to do it all and be everything to everyone, but keeping nourished should be a top priority. In the previous parts of this series, we examined mothers’ challenges with producing adequate milk supply for their babies, as well as nutrition and supplements to support her supply. Motherhood and liquid gold Proper diet and hydration are often sacrificed when juggling the demands of a new baby, housework, career, other children, and any semblance of a social life. This altruistic sacrifice could unknowingly lead to negative consequences. Milk Production 101 While the need for nutrient-dense foods will always ring true, the number of calories required to allow healing and support adequate milk production varies from woman to woman. Calorie needs for breastfeeding moms depend on how much energy mom is exerting daily, plus how much milk she is producing. On average, an exclusively breastfeeding mother needs about 500-640 calories more per day than she did prepregnancy.1,2 The average baby consumes 19-30 ounces of milk per day, but mother’s hydration needs actually exceed the amount of milk produced and her prenursing hydration needs combined.3 According to the Dietary Reference Intakes (DRIs), mom needs around an extra 34 ounces (1 liter) of water each day, and if she still feels thirsty, she should drink more water.4 Fueling the nurturer It’s common for new moms to fall into the habit of always putting baby first. Of course, it’s important to keep baby out of harm’s way, but when baby’s needs are met, it’s okay to put baby down (or wear baby in carrier) so that mom can put on her own proverbial oxygen mask. The act of growing a baby and then giving birth is a tremendous stressor on a woman’s body. Albeit a completely natural, beautiful, and often relished stressor, a women’s body needs rest and nutrient-dense foods to heal properly and to continue to give life to her baby. Across various traditional cultures, there are heavy emphases on postpartum nutrition. While the dishes for postpartum nutrition vary by culture, there are many commonalities, with animal products, cooked vegetables, herbs, and spices as mainstays in most cultures.5 Eating to heal At a glance, traditional healing foods reveal that broths, soups, stews, and porridge are central to a new mother’s diet.6 Slow-cooked stews and broths are rich in collagen-building amino acids such as glycine and proline, electrolytes, and “warming” spices and herbs.5 Porridge-like foods and cooked vegetables provide fiber-rich carbohydrates. It’s no coincidence that these nutrient-dense foods are easy to digest and rich in iron, B vitamins, zinc, choline, DHA, protein, carbohydrates, and a number of other nutrients that support replenishing red blood cells, tissue healing, and the production of high-quality breastmilk.5 In addition to eating wholesome foods, new mothers should not reduce calories or carbohydrates in the months immediately following giving birth.7-9 If weight loss is desired once her breastmilk supply is established, mom can mindfully reduce carbohydrate intake while monitoring her milk supply and ensure her diet remains otherwise nutrient-dense.5 Nourishing baby Like adult food, human milk is made up of carbohydrates, fat, protein, vitamins, and minerals, plus the addition of nonnutritive bioactives. Some of the milk components remain at consistent levels across the breastfeeding relationship, while others vary from mother to mother and for each mother across time.10 Each mother’s milk is unique based on her dietary intake, body stores, time frames (time of day, season, circadian rhythms), time intervals (time of day, time since previous breast emptying and duration of feed), and time relative to maternal exposures (e.g., meals, pathogens, and supplements).10,11 Let’s explore these nutrients a little further… Fat Breastmilk fat quantity is mainly dependent on the feeding period, the stage of the feed, and the number of pregnancies mom has had, while maternal diet (energy intake, amount of dietary fat) and lifestyle are less relevant (except in cases of severe malnutrition).12 Fat is made up of subunits called fatty acids; the fatty acid profile of breastmilk is reliant upon both mom’s current diet and her dietary intake during the pregnancy.13 Interestingly, much of the fat in early breastmilk comes from mom’s longer-term food intake, mainly during the third trimester of pregnancy.13 And while the amount of fat in breastmilk is not directly related to diet, the composition of the fatty acids in the breastmilk is related to diet.13 Important to fetal and infant brain and vision development, eicosapentaenoic acid (EPA) and docosahexanoic acid (DHA) are two omega-3 fatty acids that may be lacking in mom’s diet. If she consumes a standard American diet (SAD) or a vegan diet, which are inherently lacking in fatty fish intake, baby is at an especially high risk of deficiency.14 Even though the human body holds the necessary enzymatic pathway to make DHA from its plant-based precursor alpha-linolenic acid (ALA), there is clear evidence that the conversion of ALA to EPA and DHA is insufficient to ensure adequate levels in baby.17 In fact, it has been shown that the efficiency of the conversion of ALA to EPA is lower than 10%; the conversion of ALA to DHA is even lower, and virtually nonexistent in boys and men.15 Pregnant and lactating women should aim to consume an average dietary intake of at least 200 mg DHA/d.16 In order to balance adequate amounts of EPA and DHA with lowered risk of environmental contaminants, more small fish (e.g., sardines, anchovies and mackerel) should be eaten over larger fish, and wild-caught or safely farmed salmon should also be preferred. Fortunately, nature has included selenium in fatty fish, which counteracts methylmercury toxicity in humans and protects against some neurological effects of mercury exposure.17 This is an important fact to note in light of weighing the risks to benefits of increased seafood intake with increasing exposure to harmful methylmercury, polychlorinated biphenyls (PCBs), and dioxins found in some seafood.18 Supplementation with DHA and EPA that has been third party-tested for contaminants (e.g. heavy metals, dioxins, etc.) can be a convenient way for mothers to ensure adequate omega-3 fatty acid intake. Protein Like fats, the protein composition of human milk is more affected by mother’s intake than the actual amount of protein in the milk or by maternal or gestational age.10 While the concentration of protein in the milk is not affected by mom’s diet, it does increase with maternal body weight for height and decreases in mothers producing higher amounts of milk.19 In addition, while the makeup of breastmilk shows a consistent level of protein regardless of time of day, although protein concentration does decrease through each lactation session.20 Carbohydrates The predominant carbohydrate in breastmilk is lactose; however, there are also nondigestible, nonnutritive carbohydrates. These nondigestible carbohydrates, called oligosaccharides, act as food for the beneficial gut bacteria that bloom into baby’s gut microbiome.10 Lactose concentrations are lowest in colostrum and increase through the first 4 months of lactation.21 Unlike the other macronutrients, lactose concentrations are fairly consistent across the milk of different mothers and are not influenced by maternal weight or number of pregnancies.10 Vitamins and minerals As mentioned earlier, some nutrients depend on mom’s current dietary intake, while others rely on her bodily stores.10 The following nutrients change with mother’s intake, adequacy or deficiency, and/or supplementation. Real food sources follow each nutrient:11,23
It’s important to note that it’s difficult to consume adequate vitamin D through food alone. Known as the “sunshine vitamin,” vitamin D is mostly obtained through unprotected skin’s exposure to ultraviolet (UV) light, but in geographic areas with poor seasonal UV exposure or in individuals who spend a lot of time indoors, supplementation may be necessary. Fortunately, a new randomized controlled trial found that for deficient mothers, supplementing with 6,000 IU of vitamin D3 safely optimizes maternal vitamin D status and improves milk vitamin D to maintain adequate infant serum vitamin D levels.24 Vitamin D levels should be monitored by a healthcare practitioner. Final thoughts… Breastmilk conveys immeasurable benefits, even if some of the nutrients are lacking at times, and is therefore baby’s preferred food.24 That said, fed is always best. References 1. Institute of Medicine (US) Committee on Nutritional Status During Pregnancy and Lactation. Nutrition During Lactation. Washington (DC): National Academies Press (US); 1991. 9, Meeting Maternal Nutrient Needs During Lactation. https://www.ncbi.nlm.nih.gov/books/NBK235579/ 2. Kominiarek MA et al. Nutrition recommendations in pregnancy and lactation. Med Clin North Am. 2016;100(6):1199–1215. 3. Dewey KG et al. Milk and nutrient intake of breast-fed infants from 1 to 6 months: relation to growth and fatness. J Pediatr Gastroenterol Nutr. 1983;2(3):497-506. 4. “‘Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate’ at NAP.edu.” National Academies Press: OpenBook, 2005, www.nap.edu/read/10925/chapter/1. 5. Nichols L. Real Food for Pregnancy. United States;2018:222-238. 6. Raman S et al. Eating soup with nails of pig: thematic synthesis of the qualitative literature on cultural practices and beliefs influencing perinatal nutrition in low and middle income countries. BMC Pregnancy Childbirth. 2016;16(1):192. 7. Sloan G et al. A rare cause of metabolic acidosis: ketoacidosis in a non-diabetic lactating woman. Endocrinol Diabetes Metab Case Rep. 2017;2017. pii: 17-0073. 8. Al Alawi AM et al. Lactation ketoacidosis: case presentation and literature review. BMJ Case Rep. 2018;2018. pii: bcr-2017-223494. 9. Gleeson S et al. Lactation ketoacidosis: an unusual entity and a review of the literature. Perm J. 2016;20(2):71–73. 10. Dror DK et al. Overview of Nutrients in Human Milk. Adv Nutr. 2018;9(suppl_1):278S-294S. 11. Casavale KO et al. NIH workshop on human milk composition: summary and visions. Am J Clin Nutr. 2019. pii: nqz123. doi: 10.1093/ajcn/nqz123. [Epub ahead of print] 12. Sauerwald TU et al. Polyunsaturated fatty acid supply with human milk. Lipids. 2001;36(9):991-996. 13. Mennitti LV et al. Type of fatty acids in maternal diets during pregnancy and/or lactation and metabolic consequences of the offspring. J Nutr Biochem. 2015;26:99–111. 14. Bzikowska-Jura A et al. The concentration of omega-3 fatty acids in human milk is related to their habitual but not current intake. Nutrients. 2019;11(7):1585. 15. Marangoni F et al. Maternal diet and nutrient requirements in pregnancy and breastfeeding. An Italian consensus document. Nutrients. 2016;8(10):629. 16. Koletzko B et al. Perinatal Lipid Intake Working Group; Child Health Foundation; Diabetic Pregnancy Study Group; European Association of Perinatal Medicine; European Association of Perinatal Medicine; European Society for Clinical Nutrition and Metabolism; European Society for Paediatric Gastroenterology, Hepatology and Nutrition, Committee on Nutrition; International Federation of Placenta Associations; International Society for the Study of Fatty Acids and Lipids. Dietary fat intakes for pregnant and lactating women. Br J Nutr. 2007;98(5):873-877. 17. Mania M et al. [Fish and seafood as a source of human exposure to methylmercury]. Rocz Panstw Zakl Hig. 2012;63(3):257-264. 18. Mozaffarian D et al. Fish intake, contaminants, and human health: evaluating the risks and the benefits. JAMA. 2006;296(15):1885-1899. 19. Nommsen LA et al. Determinants of energy, protein, lipid, and lactose concentrations in human milk during the first 12 mo of lactation: the DARLING Study. Am J Clin Nutr. 1991;53(2):457-465. 20. Hollanders JJ et al. The association between breastmilk glucocorticoid concentrations and macronutrient contents throughout the day. Nutrients. 2019;11(2):259. 21. Coppa GV et al. Changes in carbohydrate composition in human milk over 4 months of lactation. Pediatrics. 1993;91(3):637-641. 22. Micronutrient Information Center. Linus Pauling Institute. https://lpi.oregonstate.edu/mic. Published 2019. Accessed August 28, 2019. 23. Dawodu A et al. The effect of high-dose postpartum maternal vitamin D supplementation alone compared with maternal plus infant vitamin D supplementation in breastfeeding infants in a high-risk population. A randomized controlled trial. Nutrients. 2019;11(7). pii: E1632. 24. Zhu J et al. The Functional Power of the Human Milk Proteome. Nutrients. 2019;11(8). pii: E1834. Did you know your hormones affect your urinary tract and vaginal health?* Before menopause, your hormones rise and fall with your menstrual cycle, causing you to be more likely to develop an imbalance in your vaginal microbiome in the two weeks following the beginning of your period.1 Additionally, the hormonal shifts that come with perimenopause and menopause also affect urinary tract comfort.2 As well, disruption to your hormone levels may also cause a range of symptoms like PMS;3 heavy or light periods;3 tender or swollen breasts;4 weight gain around the butt, hips, waist, and back of arms;5-7 low mood; anxiousness; fatigue;7 and reduced libido.7 Here are some foods to eat and others to avoid to help keep your hormones in harmony: Another way to ensure you’re getting the nutrients you need to support your health is to add supplements like Wellness Essentials® Women or Wellness Essentials Women’s Prime to your daily regimen.
For additional urinary tract and vaginal health, consider taking a probiotic specific to urinary tract and vaginal health.* References
By Monazza Ahmad, B.Pharm, MSc
A healthy genital tract makes some of the most important phases in a woman’s life more enjoyable and easier to manage. Menstruation, intimacy, giving birth, and embracing menopause are all significant milestones. But you may not realize that good vaginal health plays a fundamental role in reaching these milestones with minimum hurdles. Importance of gut health is well-researched and well-understood for our overall health, concluding that the gut is vital to the health of most organs in our body. Gut health is defined by the microbiome that resides in it and influences the absorption and digestion of everything we consume. These microorganisms constantly and selectively translocate to different parts of the body, creating a unique microecosystem in each organ.1 Curious how the vaginal microbiome differentiates from the gut microbiome? To understand this concept better, we will briefly explore the diversity of the microbiome in the human body. Diversity of human microbiomeMicrobiome diversity in our body depends on factors like diet, environment, genetics, and early exposure to microbiota, meaning at birth. Just like skin and scalp, the female genital tract is also represented by its own community of microorganisms. The vaginal microbiota is evolved through a continuous translocation of species from gut to vagina or from a mother to child at birth.1 Driven by hormonal changes, the complex vaginal microbiome is continuously transformed throughout various cycles of the female lifetime—from birth to puberty, menstruation, pregnancy, menopause, and postmenopause.1 Difference between gut and vaginal microbiomeSimply put, gut microbiota is more diverse while vaginal microbiota is more selective in healthy bacterial strains. This means using the same interventions to protect vaginal flora as that for the gut may not always be optimal. Recognizing the difference between the native microbiome of gut and vagina helps us find the right and safe solutions to help avoid undesirable genital conditions.1 It is important to understand that the physiological and biochemical characteristics of microorganisms remain the same in the gut and vagina; however, their immune responses vary considerably between the two environments.1 In other words, the way each environment detects a substance as harmful or safe is different.1 For example, where the by-products of bacterial fermentation (such as short-chain fatty acids) have shown to prevent damage to the gastrointestinal tract, they have shown unfavorable effects in the genital tract, leading to negative outcomes in the reproductive and gynecological system.1 When the undesirable bacteria from the gut invade the vaginal or urethral area, they create an imbalance that may lead to various female concerns. What is the gut-vagina axis?Modern research has revealed a collection of intricate pathways, namely gut-vagina axis, which connects the vaginal tract to our gut. Despite the difference between intestinal flora and the vaginal flora, the former is found to be involved in the development of some vaginal imbalances. For example, bacteria from the gut pass to the rectum, from where they can travel to the vagina due to the close proximity, resulting in unfavorable conditions. Therefore, it is important to keep the communication smooth between the gut and vagina.2 Effects of vaginal microbial imbalanceVaginal microbial imbalances may result in several unfavorable conditions.
Factors affecting the vaginal microbiomeThe intricate and dynamic female genital tract requires special attention to care. Here are some of the factors that can create imbalance in the vaginal microbiome.
References: 1. Amabebe E et al. Front Immunol. 2020;11:2184. 2. Brannon JR et al. Nat Commun. 2020;11:2803. 3. Han Y et al. Front Micriobiol. 2021;12:643422. 4. Lehtoranta L et al. Front Micriobiol. 2022;13:819958. 5. Gholiof M et al. Front Reprod Health. 2022;4:963752. 6. Lewis FMT et al. Obstet Gynecol. 2017;129(4):643–654. 7. Cheng G et al. Eukaryot Cell. 2006;5(1):180–191. 8. Mirmonsef P et al. PLoS One. 2014;9(7):e102467. 9. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/yeast-infection/symptoms-causes/syc-20378999. Accessed December 5, 2022. 10. Gupta K et al. J Infect Dis. 2000;181(2):595-601. 11. Szymański JK et al. Int J Environ Res Public Health. 2021;18(9):4935. 12. Neggers YH et al. J Nutr. 2007;137(9):2128-2133. 13. Tohill BC et al. Am J Clin Nutr. 2007;85(5):1327-1334. |
Categories
All
Archives
April 2024
|
|
Join Our Community
|
|
Amipro Disclaimer:
Certain persons, considered experts, may disagree with one or more of the foregoing statements, but the same are deemed, nevertheless, to be based on sound and reliable authority. No such statements shall be construed as a claim or representation as to Metagenics products, that they are offered for the diagnosis, cure, mitigation, treatment or prevention of any disease. PAIA Manual |












 RSS Feed
RSS Feed