|
by Ashley Jordan Ferira, PhD, RDN
A food fortification trial demonstrated that 600 IU of daily vitamin D3 had a significantly greater impact than 600 IU of daily vitamin D2 in elevating serum blood levels of 25-hydroxyvitamin D [25(OH)D].1-2 Vitamin D is essential for skeletal health and many emerging extraskeletal physiological processes, but remains one of the most common micronutrient dietary gaps, resulting in widespread hypovitaminosis D globally. Understanding how much vitamin D the body needs daily, in what form, and from what sources is still being discovered. There are two forms of vitamin D: plant-based ergocalciferol (vitamin D2) and animal-based cholecalciferol (vitamin D3). D2 can be found in UV-irradiated mushrooms, certain fortified foods (breakfast cereals, margarine, and milk), dietary supplements, and vitamin D prescription medications. D3 is found in oily fish, egg yolks, fortified milk, and dietary supplements.4 Chemically, D2 and D3 are almost identical except for key side chain differences, with D2 having an additional double bond. D3 has been shown to have a higher affinity to the vitamin D binding protein, hepatic 25-hydroxylase (enzyme that converts vitamin D to the circulating 25(OH)D form) and vitamin D receptor. Whether these chemical and cellular differences translate into differential abilities in raising serum 25(OH)D, the clinical measure of vitamin D status, has been a hotly debated topic since the early 20th century.5 Research literature to date demonstrates a robust case gaining momentum for vitamin D3 and against vitamin D2 for supplementation.4-5 In particular, a 2012 systematic review and meta-analysis by of randomized controlled vitamin D supplementation trials in humans explored a head-to-head comparison of vitamin D2 vs. D3 in raising serum 25(OH)D; vitamin D3 was clearly shown to be more efficacious at raising and maintaining serum 25(OH)D levels than vitamin D2.4 Authors concluded that vitamin D3 may be considered the preferred choice for supplementation.4 Since natural sources of vitamin D (dietary input and UVB exposure from the sun) are limited, and a daily vitamin D supplementation regimen is a personal health decision, vitamin D fortification of the food supply is an important, strategic public health measure to help increase dietary vitamin D intake and improve status in the general population.6 Clarity is needed to elucidate whether D2 and D3 are equally effective sources for food fortification, since both forms are currently utilized in the food supply.6 A study by Tripkovic et al. helps to shed light on key differences.1 Results were published in The American Journal of Clinical Nutrition by Dr. Laura Tripkovic and colleagues from a randomized, double-blind, placebo-controlled food fortification trial that included 335 healthy South Asian and white European women aged 20–64 years.1 Participants were randomized to one of five groups: 1) Placebo: Placebo juice with placebo biscuit 2) D2J: Juice supplemented with 15 mcg vitamin D2 with placebo biscuit 3) D2B: Placebo juice with biscuit supplemented with 15 mcg vitamin D2 4) D3J: Juice supplemented with 15 mcg vitamin D3 with placebo biscuit 5) D3B: Placebo juice with biscuit supplemented with 15 mcg vitamin D3 Fifteen mcg of vitamin D is equivalent to 600 IU of vitamin D, which is the US Recommended Daily Allowance (RDA) for ages 1-70 years.7 The daily food-fortified intervention was 12 weeks long during the winter, and serum total 25(OH)D levels were collected at baseline, week 6 and week 12. Data analysis combined ethnic groups. D3-fortified consumption was shown to be twice as effective as D2 in raising 25(OH)D serum levels in the body.1 While the placebo group experienced a 25% reduction in serum 25(OH)D levels over the course of the study, the D2J and D2B groups saw 25(OH)D increases of 33% and 34%, respectively. Most effective, however, were the D3 groups, with 25(OH)D increases in the D3J and D3B groups of 75% and 74%, respectively. The D3J group induced higher incremental increases in 25(OH)D levels: 16.9 nmol/L higher than the D2J group, 16.0 nmol/L higher than the D2B group, and 42.9 nmol/L higher than the placebo group.1 Both juice- and biscuit-supplemented vitamin D3 groups demonstrated similar results, with no statistical differences seen between D3J and D3B groups.1 Compared to white European women, the South Asian women demonstrated a greater increase in 25(OH)D levels in response to both D2 and D3, which was likely caused by their lower baseline vitamin D status.1 This study shows that modest supplementation levels (600 IU daily) of D3 in food and beverage sources twice as effective at raising serum levels of 25(OH)D than vitamin D2.1This study and previous supplementation studies may impact future policy and practice for vitamin D supplementation source. Additional research addressing dose response, bioactivity of D3 versus D2 and the impact of foods with high levels of vitamin D3 is needed.2 Why is this Clinically Relevant?
Link to abstract Citations
0 Comments
The female-centric 411 on this essential nutrientby Ashley Jordan Ferira, PhD, RDN
Overview Vitamin D research and daily news headlines are ubiquitous. PubMed’s search engine contains over 81,800 articles pertaining to vitamin D.1 Information abounds on vitamin D, but the vetting and translation of that information into pragmatic recommendations is harder to find. Evidence-based takeaways and female-centric recommendations are crucial for healthcare practitioners (HCPs), their female patients and consumers alike. Women are busy, multi-tasking pros, so practical, personalized takeaways are always appreciated. In other words, women need the “411” on vitamin D. Merriam-Webster defines “411” as “relevant information” or the “skinny”.2 So for all of you busy women, here’s the skinny on vitamin D. Let’s explore common questions about this popular micronutrient. Q: Is vitamin D more important for younger or older women? A: All of the above. Vitamin D plays a critical role in women’s health across all life stages, from fertility/conception, to in utero, childhood, adolescence, adulthood, older adulthood, and even in palliative care. Vitamin D is converted by the liver and kidneys into its active hormone form: 1,25-dihydroxyvitamin D. This dynamic hormone binds nuclear receptors in many different organs in order to modulate gene expression related to many crucial health areas across the lifecycle, including bone, muscle, immune, cardiometabolic, brain, and pregnancy to name a few.3 Q: I am a grandmother. Are my vitamin D needs different than my daughter and granddaughter? A: Yes, age-specific vitamin D recommendations exist. As an essential fat-soluble vitamin, women need to achieve adequate levels of vitamin D daily. Age-specific Recommended Dietary Allowances (RDA) from The Institute of Medicine (IOM),4 as well as newer clinical guidelines from The Endocrine Society,5 provide helpful clinical direction for daily vitamin D intake and/or supplementation goals. The IOM RDAs4 are considered by many vitamin D researchers to be a conservative, minimum daily vitamin D intake estimate to support the bone health of a healthy population (i.e. prevent the manifestation of frank vitamin D deficiency as bone softening: rickets and osteomalacia): Infants (0-1 year): 400 IU/day Children & Adolescents (1-18 years): 600 IU/day Adults (19-70 years): 600 IU/day Older Adults (>70 years): 800 IU/day The Endocrine Society’s clinical practice guidelines5 recommend higher daily vitamin D levels than the IOM, with a different end-goal: raising the serum biomarker for vitamin D status [serum 25-hydroxvitamin D: 25(OH)D] into the sufficient range (≥ 30 ng/ml) in the individual patient: Infants (0-1 year): At least 1,000 IU/day Children & Adolescents (1-18 years): At least 1,000 IU/day Adults (19+ years): At least 1,500 – 2,000 IU/day Q: I am a health-conscious woman who eats a nutritious, well-rounded diet. I should not need a vitamin D supplement, right? A: Not so fast. Daily micronutrient needs can be met via diet alone for many vitamins and minerals. Vitamin D is one of the exceptions, which is why an alarming number of Americans (93%) are failing to consume the recommended levels from their diet alone.6-7 Very few foods are endogenous sources of animal-derived vitamin D3 (cholecalciferol) or plant-derived vitamin D2 (ergocalciferol). Some natural vitamin D sources include certain fatty fish (e.g. salmon, mackerel, sardines, cod, halibut, and tuna), fish liver oils, eggs (yolk) and certain species of UV-irradiated mushrooms.8 In the early 20th century, the US began fortifying dairy and cereals with vitamin D to help combat rickets, which was widespread. For example, one cup (8 fluid ounces) of fortified milk will contain approximately 100 IU of vitamin D. Even though some food sources do exist, the amounts of these foods or beverages that an adult would need to consume daily in order to achieve healthy 25(OH)D levels (> 30 ng/ml) is quite unrealistic and even comical to consider. For example, you would need to toss back 20 glasses of milk daily or 50 eggs/day to achieve 2,000 IU of vitamin D! In contrast, daily vitamin D supplementation provides an easy and economical solution to consistently achieve 2,000 IU and any other specifically targeted levels. Q: I enjoy the outdoors and get out in the sun daily, so I should be getting all of the vitamin D that I need, correct? A: Vitamin D is a highly unique micronutrient due to its ability to be synthesized by our skin following sufficient ultraviolet (UV) B irradiation from the sun. Many factors can result in variable UV radiation exposure, including season, latitude, time of day, length of day, cloud cover, smog, skin’s melanin content, and sunscreen use. Furthermore, medical consensus advises limiting sun exposure due to its established carcinogenic effects. Interestingly, even when dietary and sun exposure are both considered, conservative estimates approximate that 1/3 of the US population still remains vitamin D insufficient or deficient.9 Q: What factors can increase my risk for being vitamin D deficient? Are there female-specific risk factors? A: Although the cutoff levels for vitamin D sufficiency vs. deficiency are still debated amongst vitamin D researchers and clinicians, insufficiency is considered a 25(OH)D of 21-29 ng/ml, while deficiency is < 20 ng/ml.5 Therefore, hypovitaminosis D (insufficiency and deficiency, collectively) occurs when a patient’s serum 25(OH)D falls below 30 ng/ml. The goal is 30 ng/ml or higher. Ideally, vitamin D intake recommendations4-5 and therapy are personalized by the HCP based on patient-specific information, such as baseline vitamin D status, vitamin D receptor single nucleotide polymorphisms and other pertinent risk factors. Common risk factors for vitamin D deficiency to look out for include: -> Overweight/obesity -> Older age -> Regular sunscreen use -> Winter season -> Frequent TV viewing -> Dairy product exclusion -> Darker skin (more melanin) -> Not using vitamin D supplements -> Malabsorption disorders (e.g. bariatric surgery, IBD, cystic fibrosis) -> Liver disease -> Renal insufficiency -> Certain drug classes: weight loss, fat substitutes, bile sequestrants, anti-convulsants, anti-retrovirals, anti-tuberculosis, anti-fungals, glucocorticoids -> Lastly, additional female-specific risk factors to look out for include exclusive breastfeeding while mother is vitamin D insufficient (can result in infant being vitamin D deficient) and certain cultural clothing that covers significant amounts of skin surface area (e.g. hijab, niqab). Key Takeaways
Food first, but fill the gap: The case for vitamin D supplementationAshley Jordan Ferira, PhD, RDN
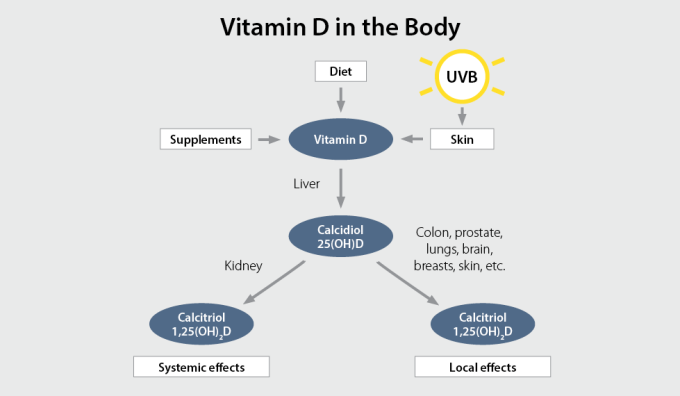
If you can have a favorite nutrient, mine would be vitamin D. Historically famous for its essential, classical role in calcium and phosphorus homeostasis and bone physiology (think rickets prevention), the past few decades of research have unveiled diverse, extraskeletal health roles for vitamin D, including but not limited to the immune system, cardiometabolic pathophysiology, cancer, pregnancy, etc. Whether consuming vitamin D2 or D3 (FYI, the latter more potently impacts vitamin D status),1 vitamin D ultimately circulates in the 25-hydroxyvitamin D [25(OH)D] form (the clinical biomarker used to measure vitamin D status) and acts throughout the body as a pleiotropic hormone in its active form, 1,25-dihydroxyvitamin D [1,25(OH)2D]. Unlike other nutrients, this fat-soluble vitamin is obtainable via several unique routes: the skin with adequate UVB exposure, a handful of natural food sources, a few fortified foods, dietary supplements, and even prescription drugs. The problem is that few foods naturally contain vitamin D (e.g., egg yolk, certain fatty fish, fish liver oil, and certain species of UV-irradiated mushrooms), and fortified foods offer relatively small amounts (e.g., 100 IU vitamin D per 8 oz cup of fortified milk or orange juice),2 so vitamin D supplementation becomes a strategic solution. In the eloquent words of pediatrician and vitamin D researcher, Carol Wagner, MD: “Something so simple- vitamin D supplementation- could improve the health status of millions and so becomes an elegant solution to many of our health problems today.” If it’s possible to be defensive of a micronutrient, I am protective of vitamin D. Non-evidence-based rumors and negative media attention targeting vitamin D are common. Some of the misinformation is hype from anti-supplement camps who make broad, sweeping statements that lack scientific substantiation. But not all of the vitamin D myths originate from bias or lack of intellectual rigor. After all, who has time to keep up with the impressive, daily output of new vitamin D research? Clinicians certainly do not have the luxury of time, not in the current healthcare paradigm. Nevertheless, when inaccurate conclusions are propagated to patients about vitamin D and their health, that’s more harm than good. So, let me help out. This blog series explores some of the most common vitamin D myths. Let’s tackle just 1 myth today: Myth: I get enough vitamin D from food, so I don’t need a vitamin D supplement. Can you meet your vitamin D needs from food alone? Well, that depends on how you define “needs.” Let’s talk about the 2 major (and quite different) sets of vitamin D recommendations. First, the National Academy of Medicine (NAM), formerly known as the Institute of Medicine, provided vitamin D Recommended Dietary Allowances (RDAs) in 2010.3 Here’s how much vitamin D NAM says that we (Americans and Canadians) need based on bone health research (think rickets and osteomalacia prevention, calcium absorption, etc.):3
But I have a bone to pick (pun intended) with NAM’s vitamin D recommendations. I find them to be problematic, if not contradictory at times, for a few key reasons. To start with, the RDA is by definition “the average daily level of intake sufficient to meet the nutrient requirements of nearly all (97-98%) healthy people.”4 Well, that misses the unhealthy people. Since 2/3rd of the country are overweight or obese5 and heart disease and cancer are the #1 and #2 causes of mortality in the US, respectively,6 one can extrapolate that the vitamin D RDAs do not apply to a decent chunk of the gen pop. In fact, research indicates that overweight and obese individuals require more vitamin D than their lean counterparts,7 but the NAM recommendations fail to consider adiposity. Second, lumping a toddler and 68-year-old grandmother in the same RDA category (i.e., ages 1-70 years) seems to lack nuance. Skeletal health is critical throughout life, but you cannot tell me that the vitamin D needs for the rapidly accruing skeleton in childhood and adolescence are no different than an adult or older adult’s skeletal needs. Third, the RDAs for daily vitamin D intake are simply incongruent with the serum 25(OH)D cutoffs NAM also published in 2010. They provided the following 25(OH)D ranges:
In the sage words of the late Bob Heaney, MD: “We’ve been able to show that the (vitamin D) RDA barely budges the blood 25-hydroxyvitamin D level.”8 Thanks to Dr. Heaney, who made invaluable research contributions to the field of vitamin D, we know that 100 IU/day of vitamin D increases serum 25(OH)D concentrations by approximately 1 ng/mL.9 That means that 1,000 IU/day of vitamin D would raise 25(OH)D by about 10 ng/mL. Although weight status, age, and the patient’s baseline vitamin D status can variably impact the supplementation response, this “rule of thumb” can be used to roughly calculate vitamin D supplementation needs. For example, let’s take a patient: me. I have limited UVB sun exposure and consume some foods that contain vitamin D (e.g., milk, eggs, salmon) but irregularly. My daily 5,000 IU vitamin D3 supplement has my serum 25(OH)D at 54 ng/mL. It stays between 50-60 ng/mL, which is in the sufficient range. But I’m an anomaly. Nationally representative research backs up the fact that Americans are not getting adequate vitamin D from their diets.10-11 First, 93% of Americans 2 years and older are failing to consume at least 400 IU/day of vitamin D from diet alone, and this estimate includes fortified food sources.10 Even when diet plus sun exposure are both thrown into the mix, about 1/3rd of the US population has serum 25(OH)D levels associated with vitamin D insufficiency or deficiency.11 For more details on vitamin D deficiency and why it persists, check out this blog. Dietitians (I am one) and other clinicians love to preach “food first.” That slogan is true but ignores research on key nutrient gaps. I prefer to say, “food first, then fill the gaps.” And in the case of vitamin D, the gap is practically guaranteed, except for the outlier patient who’s knocking back fish liver oils and irradiated mushrooms. Lastly, a more current and scientifically and clinically nuanced set of guidelines exist. One year after the NAM recommendations were released, several of the world’s leading vitamin D researchers convened to review the evidence to date, resulting in the 2011 publication: Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline.12 The US Endocrine Society’s conclusions are harmonious with the mindset of a clinician, who is tasked with addressing the vitamin D needs of unique patients. The guideline recommends higher daily vitamin D levels than NAM, with a different and logical purpose in mind: Raising serum 25(OH)D levels into the sufficient range (≥ 30 ng/ml):12
Individual genetic differences for the vitamin D receptor (VDR) (i.e., gene polymorphisms like Cdx2, Apa1, Fok1, Taq1) are another important facet to weave into each patient’s unique vitamin D story, underscoring the prudence of a personalized lifestyle medicine approach to treat the individual. Takeaway: No, you cannot satisfy your vitamin D needs from food alone. If you plan to raise and maintain your serum 25(OH)D level (the biomarker that indicates vitamin D status) in the sufficient range for skeletal and extraskeletal health, that will require daily vitamin D supplementation. Remember, 30 ng/mL is not the goal. It’s the cutoff for insufficiency. Here’s a sneak peak at some of the additional vitamin D myths that will be covered in future blogs:
Citations
Did you know that getting just 10 minutes of sunshine (ultraviolet B, or UVB) per day helps the body create approximately 10,000 IU of vitamin D?1 This nutrient is necessary for the health of your bones, as well as overall health.2 However, during the months of November through February, and if you live north of Atlanta, there won’t be enough UVB rays to penetrate through the atmosphere and help your skin generate this vital nutrient. So is there something you can do? Sometimes you just have to create your own sunshine. And considering that three-quarters of teens and adults in the United States are deficient in vitamin D,3 as well as 1 billion people worldwide,4 this is where supplemental vitamin D can really help. Natural dietary sources of vitamin D are few (e.g. fatty fish, eggs), and fortified dietary sources such as milk, orange juice and cereal provide minimal amounts of vitamin D. This is why vitamin D is one of the most common nutrient gaps and also one of the easiest to address via supplementation. Why is vitamin D important? Vitamin D is a fat-soluble vitamin that regulates bone growth and mineralization and plays an important role in ensuring the muscles, heart, lungs, and brain function properly.2 Vitamin D has also been shown to support immune function. Vitamin D is not only an essential vitamin but also acts as a hormone in the body. Vitamin D that you obtain from the sun, food, beverage, or supplements must be first activated by the liver which converts the vitamin D to 25-hydroxyvitamin D (25(OH)D), also known as calcidiol.2 It is then converted by the kidneys and target tissues in the body to the biologically active form 1,25-dihydroxyvitamin D (1,25(OH)2D), also known as calcitriol.2 Calcitriol is the active, hormone form, which supports a variety of physiological functions, including helping the body regulate levels of calcium and phosphorus, as well as mineralize bone.5 Vitamin D deficiency What does it mean to be deficient in vitamin D? Measuring serum concentrations of 25(OH)D rather than 1,25(OH)2D is a better indicator of vitamin D status in the body due to its longer half life. Certain groups define vitamin D deficiency as 25(OH)D level less than 20 ng/mL (50 nmol/L).6 Vitamin D deficiency can be an issue for many people, including:7
Finding out if you need more vitamin D Measuring your vitamin D levels via a blood test is the only way to definitively know if you’re getting enough of this nutrient. With a 25(OH)D blood test from your healthcare practitioner, you will know your vitamin D levels and whether you need to take a supplement. Optimal levels of vitamin D vary according to different scientific organizations. For example, for adults the Vitamin D Council recommends daily supplementation with 5,000 IU of vitamin D3 when you cannot get enough sun to achieve a status between 40-60 ng/ml; whereas, the Endocrine Society recommends 1500-2000 IU/day.7-8 Higher levels are recommended to address deficiency.8 It is also important to recheck vitamin D levels two months after beginning a supplement regimen, and adjust as needed based on your practitioner’s recommendations. Which D is right for me? It’s important to get the form of vitamin D that is most bioavailable to the body. There are two kinds of vitamin D—D2 and D3. Vitamin D2 (ergocalciferol), is found in plants such as lichens and mushrooms, which are often irradiated by growers to boost nutritional value. Some soy and almond milks are also fortified with vitamin D2. Vitamin D3 (cholecalciferol) is the natural form of this nutrient that is created by the body with sun exposure, and research has shown that the D3 form increases the total circulating level of 25(OH)D significantly more effectively than D2.9-10 Vitamin D3 is found in small amounts in oily fish such as cod and salmon, egg yolks, as well as fortified cereals and milk, and some commercial mushrooms. Additionally, vitamin D3 has been shown to maintain adequate amounts of serum vitamin D levels during the winter months.11 There are also special sunlamps to help the skin generate vitamin D, but because of the risk for skin damage from ultraviolet rays, many healthcare practitioners don’t recommend using them. Make D your favourite letter for better health Whether you’re lucky enough to get the vitamin D you need from the sun all year around, or taking a vitamin D supplement, you’re wise to ensure you get enough of this vital nutrient. If you’re wondering whether you need more vitamin D, ask your healthcare practitioner. References:
|
Categories
All
Archives
April 2024
|
|
Join Our Community
|
|
Amipro Disclaimer:
Certain persons, considered experts, may disagree with one or more of the foregoing statements, but the same are deemed, nevertheless, to be based on sound and reliable authority. No such statements shall be construed as a claim or representation as to Metagenics products, that they are offered for the diagnosis, cure, mitigation, treatment or prevention of any disease. |




 RSS Feed
RSS Feed