|
Urinary Tract Infections (UTIs) aren't just a health inconvenience; they're a global epidemic, affecting millions worldwide, with Africa bearing a particularly heavy burden of 150 million cases annually. However, amidst this alarming statistic, there's a glimmer of hope: the potential of natural solutions in tackling this pervasive issue.
The UTI Epidemic: UTIs, primarily instigated by the bacterium E. coli, pose a significant health challenge, especially for women, with half experiencing at least one UTI in their lifetime. The recurring nature of UTIs complicates treatment, often rendering conventional approaches inadequate. Harnessing Nature's Arsenal: Natural ingredients offer promising avenues in UTI management: D-Mannose: A naturally occurring monosaccharide, D-mannose emerges as a formidable weapon against UTIs. Its mechanism involves binding to E. coli bacteria, impeding their attachment to bladder walls, and facilitating their expulsion via urine. Studies highlight its superiority over antibiotics in preventing recurrent UTIs. Cranberry: Famed for its anti-adhesion properties, cranberry contains proanthocyanidins that deter E. coli attachment to urinary epithelial cells, thus diminishing infection risk. Moreover, cranberry's proanthocyanidins disrupt biofilm formation, further hindering bacterial colonization. Quercetin: This potent flavonoid boasts antioxidant and anti-inflammatory prowess, making it a valuable ally in UTI combat. Its antibacterial action, particularly against E. coli, coupled with biofilm inhibition, enhances efficacy in UTI management. Vitamin C: Beyond bolstering the immune system, vitamin C wields antibacterial effects, bolstering the body's defense against UTIs. 2’-Fucosyllactose: Derived from human milk, 2’-Fucosyllactose acts as a decoy for pathogens, thwarting their colonization and adhesion to epithelial cells in the gut—a pivotal aspect of UTI prevention. The Proof in Research: Pilot studies featuring women with UTIs showcase significant symptom and quality of life enhancements with D-mannose supplementation. Combining D-mannose and cranberry with antibiotics elevates cure rates by a remarkable 53%, underscoring the ingredients' synergistic effects. Comparative investigations between D-mannose and antibiotics for recurrent UTI prevention highlight D-mannose's superiority, offering renewed hope to recurrent infection sufferers. In Conclusion: Despite the daunting prevalence of UTIs, natural remedies offer a beacon of hope. By harnessing the potency of nature's arsenal, UTI management transcends conventional limitations. Bid adieu to UTI discomfort and embrace a journey toward wellness with nature's nurturing touch—a journey powered by D-mannose, cranberry, quercetin, vitamin C, and 2’-Fucosyllactose. References:
0 Comments
by Bianca Garilli, ND
For women, the pre- and post-menopausal years represent a time of major change in many aspects of life including spiritual, emotional, and physical. From a physical perspective, shifting levels of sex hormones such as dehydroepiandrosterone (DHEA), testosterone, and estrogen play critical roles in the transition in and through menopause. It’s during this chapter of a woman’s life that the number of ovarian follicles begin to decline. Their eventual depletion cause the ovaries to no longer respond to FSH and LH from the pituitary, resulting in cessation of estrogen and progesterone production from the ovaries.1 Declining estrogen levels typically begin several years before the final menstrual period (FMP)- which is defined as the cessation of the menstrual period for at least 1 year- and stabilize around two years after the FMP.2 In a similar fashion, testosterone levels change in women during the menopausal timeframe, although this sex hormone does not seem to experience as dramatic of a decline as estrogen. Frequently this results in a higher ratio of testosterone to estrogen in the post-menopausal timeframe.3 This higher testosterone level as compared to estrogen level has been associated with higher risk factors for cardiovascular disease (CVD) in women, although the impact on incident events of CVD, coronary heart disease (CHD), and heart failure (HF) in response to this sex hormone ratio is less clear.4 A study published in the Journal of the American College of Cardiology studied 2,834 post-menopausal women from the Multi-Ethnic Study of Atherosclerosis (MESA) cohort, with a mean age of 64.9 years and without CVD at baseline.4 Levels of testosterone, estradiol, DHEA, and sex hormone-binding globulin (SHBG) were assessed at the beginning of the study; participants were followed for an average of 12.1 years.4 Levels of sex hormones were evaluated for association with incident CVD, CHD, and HF. Adjustments were made for relevant variables including demographics, CVD risk factors, and hormone therapy use.4 The study found no associations between DHEA nor SHBG levels with incident CVD, CHD, and HF outcomes.4 However, an elevated risk for incident CVD, CHD, and HF events was found to be associated with a higher testosterone/estradiol ratio, with higher testosterone levels associated with higher CVD and CHD.4 Conversely, higher estradiol levels were associated with a lower CHD risk, leading the authors of this study to conclude that “sex hormone levels after menopause are associated with women’s increased CVD risk later in life”.4 Why is this Clinically Relevant?
View the abstract Citations
Exploring key factors associated with sleep disturbances during perimenopause by Bianca Garilli, ND
The demarcations of a woman’s physiological stages of life are often delineated by the various, unique phases and cycles associated with fertility, reproduction, and the hormones at work behind the scenes. These stages include:1
For many women, after many years of sleep deprivation during the child-bearing and rearing years, a good night’s rest is welcomed. Unfortunately, perimenopause, which typically begins sometime in a woman’s mid-to-late 40s and can last anywhere from 2-10 years, may create a whole new set of sleep challenges.2,3 Prevalence of sleep problems during perimenopause Compared to men, sleep complaints are approximately twice as prevalent in women of all ages, with a prevalence during perimenopause ranging from 39-47%, underscoring the importance of investigating sleep problems in a female-centric way.3 To this end, sleep duration and quality of a nationally representative sample of women 40-59 years of age were studied by the CDC and broken down categorically by menstrual cycle/menopausal phase; sleep data during the perimenopausal phase revealed that:4
Hormones are at play Sex hormones So what is happening during perimenopause that so dramatically and negatively impacts sleep patterns? For starters, the decline in levels of sex hormones (in particular estrogen, progesterone, and testosterone) during the perimenopausal years lead to an array of symptoms, most of which can adversely affect sleep habits. These include: hot flashes, migraines, sleep apnea, circadian rhythm abnormalities, restless legs syndrome, lifestyle factors, as well as mood disturbances such as anxiety.2,4,5 Interestingly, in an analysis reviewing sleep concerns in various stages of menses/menopause, it was found that vasomotor symptoms (hot flashes) and sleep disturbances may work bidirectionally.6 In other words, hot flashes may increase difficulties obtaining appropriate duration and quality of sleep, while sleep problems may worsen vasomotor symptoms,6 a circuitous “what came first?- chicken or egg,” kind of hormonal dance. The types of sleep disturbances most often noted by perimenopausal women include difficulties with initiating and/or maintaining sleep, as well as frequent nocturnal and/or early morning awakenings.5 It’s well known that during perimenopause, estrogen levels drop sharply, corresponding to many of the symptoms associated with this transition period. However, less well known is another hormone whose levels decline and no doubt, play a key role in sleep dysfunction. That hormone is melatonin, which decreases during perimenopause, although the decline in melatonin is more gradual than that of estrogen.7 Melatonin Melatonin secretion from the pineal gland drops as individuals hit their mid-life years, coinciding with the perimenopausal phase in women.7 An article published in the Journal of Sleep Disorders and Therapy indicates that exogenous use of melatonin may improve some of these sleep challenges, including the nocturnal awakenings observed during perimenopause.5 Further research indicates that the use of slow-release melatonin preparations increase total sleep time and sleep efficiency, as well as reducing sleep latency in patients with insomnia.5 Interestingly, melatonin may also play a role in the modulation of many symptoms and conditions associated with menopause, including reduction in bone density, mood disorders, fibromyalgia, and potentially even neurodegenerative diseases.7 Assuredly, much more research is needed in the area of sleep disorders, perimenopause, and related hormonal fluctuations. Sociodemographic factors Sociodemographic variables can also contribute to perimenopausal sleep disturbances:
Women who are experiencing sleep concerns should work with a healthcare practitioner trained to 1) take a deep dive into the various aspects of lifestyle that may be affecting sleep health and 2) identify and address any deleterious health consequences from inadequate sleep. These areas should encompass the full spectrum of her individual health and wellness, from a focused cardiovascular and metabolic exam, to an in-depth look into the social and emotional aspects of her life. Each of these areas is important to consider and address to effectively and safely treat sleep challenges during the perimenopausal years and beyond. Citations
Alternative and Emerging Treatments Angela Kelly, MA and Michael Stanclift, ND
This is the last installment of a three-part series on bacterial vaginosis (BV). In part one, we discussed a healthy vaginal microbiome, symptoms, and diagnostic criteria. In part two , we highlighted the risk factors that contribute to BV, the health impacts it can cause, and conventional antimicrobial treatments, along with their propensity for resistance. As we saw in part two , conventional antimicrobials often only temporarily resolve BV, and contribute to antibiotic resistance. For this reason, many patients turn to alternative treatments. In addition, new therapeutics are appearing and some show great promise. It is important to note that treatments such as boric acid, prebiotics, garlic, vaginal microbiome transplantation, Zataria Multiflora cream, vitamin C, antiseptics, and seaweed extracts have limited clinical data to support their use. However, multiple clinical trials can be found supporting the use of probiotics for the treatment of BV. Boric acid Though toxic if taken orally, boric acid administered intravaginally has been used to treat vaginal infections for over 100 years.1 It can lower the rate of BV recurrences when used as a complementary therapy to antimicrobials.2 A recent study shows the potential for boric acid as a standalone treatment for BV.3 Side effects are uncommon (< 10% of cases) but include watery discharge during treatment, vaginal burning sensations, and vaginal erythema.4 Prebiotics Prebiotics feed beneficial microorganisms. In a randomized double-blind study from 2012, a prebiotic gel containing prebiotics from the glucooligosaccharides (GOS) family was shown to quickly restore the vaginal microbiota.5 Additionally a clinical study from 2017 showed that prebiotic gels may also improve the success of BV treatments.6 Garlic A 2013 study comparing garlic tablets to oral metronidazole found that garlic tablets were as effective as metronidazole with far fewer reported side effects.7 Side effects of garlic tablets were more tolerable than metronidazole and included heartburn and nausea.7 Vaginal microbiome transplantation Vaginal microbiome transplantation (VMT) involves seeding a recipient’s vaginal microbiome with the bacteria from a healthy donor. A 2019 study of VMT successfully treated four out of five participants with intractable and recurrent BV.8 In some cases, multiple VMT treatments may be necessary.8 Zataria multiflora cream Also known as Shirazian thyme, Zataria multiflora is a plant native to Iran, Afghanistan, and Pakistan. The plant’s essential oil contains thymol and carvacrol, which have antibacterial properties.9 A 2008 clinical trial revealed Zataria multiflora vaginal cream to be as effective in treating BV as metronidazole vaginal cream.9 Adverse side effects of treatment included nausea, vaginal dryness, and burning. Vitamin C In a 2011 clinical trial it was shown that when administered intravaginally, silicon-coated vitamin C tablets were as effective as metronidazole gel in treating BV and were beneficial in preventing recurrences.10 However, not all participants were able to tolerate treatment due to itching, burning, and pain.10 Antiseptics In a study of patients with recurrent BV, Octenidine showed high initial cure rates over 87%; however, the development of bacterial resistance to Octenidine was very high with 37.5% of patients showing complete resistance at three treatments/one-year follow-ups.11 At six months the relapse rate of patients included in this study were as high as 66.6%.11 Seaweed extracts Preclinical research found that ethanol extract of green seaweed (U. Pertusa) possesses robust antimicrobial activity against G. vaginalis, which may have potential as a future treatment for BV.12 Probiotics: Lactobacillus reuteri RC-14 and Lactobaciullus rhamnosus GR-1 Probiotics are “live microorganisms which when administered in adequate amounts confer a health benefit on the host.”13 Currently, probiotics are not recommended as a standalone treatment for BV. However, supplementation with probiotics appears to be beneficial in managing BV, regardless of concurrent antimicrobial treatment.14 Probiotics are a promising complementary therapy to antimicrobials for the treatment of BV.15-20 Studies have shown that when taken orally, lactobacillus probiotics are safe and can improve the vaginal microbiota.16,21 Lactobacillus reuteri RC-14, which was first isolated from a healthy woman’s urogenital tract, can displace G. vaginalis biofilms in vitro.22Studies combining L. reuteri RC-14 and L. rhamnosus GR-1 show success in colonizing and rebalancing the vaginal microflora.16,21,23 Women treated with a combination of metronidazole, L. rhamnosus GR-1, and L. reuteri RC-14 were more than twice as likely to achieve cure than withantimicrobials alone (88% vs. 40%).15 Another study showed using tinidazole for treating BV was improved when combined with L. rhamnosus GR-1 and L. reuteri RC-14.24 In that study, researchers showed an 87.5% cure rate in probiotic group vs. 50% cure rate in the antibiotic/placebo group.24 A randomized, double-blind, placebo-controlled trial (RCT) in postmenopausal women with L. rhamnosus GR-1 and L. reuteri RC-14 as a standalone preventative therapy resulted in a shift from “indeterminate” to “normal” vaginal microbiota in 60% of the women in the probiotic group vs. 16% of women in the control group.25 Another RCT revealed that L. rhamnosus GR-1 and L. reuteri RC-14 may prevent BV infections in women with HIV.26 So how do these probiotics, which are taken orally, work to help the vaginal microbiome? L. rhamnosus GR-1 and L. reuteri RC-14 can colonize the vagina from the intestinal tract via the perineum.16,27 Lactobacilli weaken biofilms by producing lactic acid, hydrogen peroxide, bacteriocins, and antiadhesive biosurfactants.20 Biosurfactants produced by L. rhamnosus GR-1 and L. reuteri RC-14 work to disrupt the biofilms created by Gardnerella and residing multispecies anaerobes.20 This disruption allows probiotic strains to displace/crowd out pathogenic bacteria.20 L. rhamnosus GR-1 may also positively impact mucosal immunity, allowing the host to defend against pathogenic bacteria through colonization of the gut or vagina or both.16 With the low long-term cure rate of antibiotics in treating BV and the growing threat of antibiotic resistance, the use of probiotics in treating BV should continue to be explored further. Final thoughts BV infections can result in devastating physical, reproductive, and emotional health consequences for women and their partners. The high rate of recurrence underlines the need to improve the current standard of care. Finding personalized, effective, long-term solutions to BV requires ingenuity and tenacity. Emerging BV treatments offer clinicians better solutions to help patients stop the revolving door of BV. Liberating women from a cycle of recurring BV is well worth the endeavor. Citations
BV Risk Factors, Health Impacts, Current Antimicrobial Therapeutics, and Resistance Angela Kelly, MA and Michael Stanclift, ND
This is part two in a three-part series about bacterial vaginosis (BV). In part one we discussed a healthy vaginal microbiome, BV’s characteristics, and diagnostic criteria. In this section, we’ll explore risk factors for developing BV, the health impacts of it, and current conventional therapies. BV risk factors While the precise causes of BV are still being investigated, researchers have discovered the following risk factors that can contribute to its development:
Health impact of BV Although most cases of BV are asymptomatic, BV can still have devastating health consequences. Even without symptoms, BV can cause:
Current antimicrobial therapeutics and resistance Current antimicrobial therapeutics often provide only temporary relief and ultimately contribute to antibiotic resistance. BV is usually treated with metronidazole, clindamycin, or a combination of oral and intravaginal antibiotic therapies.49Occasionally other antibiotics such as rifaximin, secnidazole, and tinidazole are prescribed.49-51 A 2020 in vitro study showed clindamycin had greater initial effectiveness against G. vaginalis than metronidazole; however, clindamycin is strongly associated with antibiotic resistance.52-53 In a randomized clinical trial 17% of cases had baseline clindamycin resistance, and 53% showed resistance to it after therapy.53 Also of consideration, clindamycin has been linked to Clostridioides difficile (C. diff) colonization and pseudomembranous colitis.13,50,54 Studies demonstrate G. vaginalis and A. vaginae also show resistance to metronidazole, although to a lesser extent than clindamycin.52,55 When metronidazole is used to treat BV, it can break up the biofilm created by G. vaginalis and A. Vaginae; however, live cells can persist within the biofilm, allowing for recurrences.56 Microbial profiling shows metronidazole temporarily reduces vaginal microbial diversity, and the reestablished microbiota rarely returns to a balanced lactobacilli-dominant state.57 Treatment with metronidazole frequently causes the adverse effects of nausea, vomiting, GI disturbances, and metallic taste.54,58 Occasionally metronidazole may also cause seizures, peripheral neuropathy, transient neutropenia, and allergic reactions, including anaphylaxis.58 These findings highlight that effective and lasting treatments for BV are urgently needed. The pipeline of antibiotics continues to dwindle, and bacteria grow more resistant with the antibiotic treatment of each episode.59 The treatment of protracted or recurring cases of BV often results in a revolving door of relapses for patients.59 Identifying lasting treatments for BV that rely less on antibiotics is of the utmost urgency.60,61 BV recurrence after antimicrobials The recurrence rate following treatment of BV with antibiotics is high, with a study revealing that 58% of participants experienced a recurrence within a year and 69% returned to abnormal vaginal profiles.50,58 The high rate of recurrence appears to be multifaceted, linked to biofilms created by G. vaginalis and A. vaginae, impaired immune system response, antibiotic resistance, hygiene practices, and, according to some researchers, sexual transmission and reinfection by a woman’s sexual partner(s).60-63 Although there are variations in studies, a recent study showed improved BV recurrence rates when male partners were treated with oral and topical antibiotics. More research on the efficacy of treating sexual partners is needed.64 Having an untreated sexual partner is linked to a raised risk of recurrence of BV, although more research is needed.63,65 We can see the contributing factors for BV are multifactorial and that simple antimicrobial therapies are failing the majority of women they are prescribed to help. In our next and final installment in this series we’ll explore alternative and emerging treatments for BV, including the role of probiotics. We’ll see how a problem characterized by microbial overgrowth may ultimately need more microbes to see its resolution. Citations
The Vaginal Microbiome, BV Symptoms, and Diagnostic Criteria Angela Kelly, MA and Michael Stanclift, ND
In part one of this three-part series, we’ll discuss a healthy vaginal microbiome, symptoms, and the diagnostic criteria of bacterial vaginosis (BV). A healthy vaginal microbiome The vaginal microbiome is the lesser-known heroine of the body’s microbiomes and the first line of defense against pathogens that can cause infections.1-5 Like the gut microbiome, the vaginal microbiome is seeded from mother to daughter and the surrounding environment within 24 hours of birth.6-7Hormonal fluctuations related to puberty, the menstrual cycle, pregnancy, and menopause each contribute to the constantly changing landscape of the vaginal microbiome.8 During the reproductive years, the vaginal vault is populated by 90–95% lactobacilli in a balanced, healthy state. 9-10 Vaginal epithelial cells deposit glycogen, and the “friendly” lactobacilli ferment the polysaccharide, producing lactic acid.11 This fermentation process serves to lower vaginal pH, inhibit potentially harmful anaerobes’ growth, and discourage pathogens’ attachment to the vaginal epithelium.11 Additionally, lactobacilli produce antimicrobials such as hydrogen peroxide and bacteriocins, which deter biofilms and keep pathogenic anaerobes dormant.11 But what happens when the bacterial balance of the vagina is thrown out of whack? Bacterial vaginosis characteristics Bacterial vaginosis (BV) is the often silent, sometimes maddening, and quite common vaginal microbiome dysbiosis that affects 29.2% of women of reproductive age in the United States.12 The dysbiosis of BV is characterized by decreased “friendly” lactobacilli and an overgrowth of potentially pathogenic bacteria that may multiply to 1,000-10,000 times normal levels.13 Many studies suggest asymptomatic BV poses serious threats to reproductive and urogenital health and increases the risk of contracting and transmitting STIs.9,14-15 While the exact cause of BV is still under debate, the initial disruption of the vaginal microbiome is likely due to sexual transmission.16-17 Although with significantly lower frequency, females who have never been sexually active can also develop BV.18 BV is found globally, with higher incidences in certain countries and ethnicities.9 In the United States, Black and Mexican-American women are more likely to be affected by BV.9,19-20 Despite being the most common vaginal dysbiosis, women’s awareness of BV prior to their first infection is very low.21 Symptoms of bacterial vaginosis and diagnostic criteria While most BV cases occur asymptomatically, the CDC describes the following common symptoms that may occur:12,22
BV can be diagnosed using Amsel’s criteria or the Nugent scoring system. Amsel’s criteria for the diagnosis of BV are met when 3 out of 4 of the following clinical signs are present:23
Alternatively, the Nugent scoring system can be used to diagnose BV using a Gram stain, microscope, and a 0-10 score based on the amounts of the following microorganisms seen per high-powered field:24
So now that we have some of the basic background knowledge of the vaginal microbiome and how to detect BV in our patients, part two of this series will look at causes and risk factors, health impacts, and current conventional therapies for BV. In part three, we’ll look at alternative and emerging treatments, the role of probiotics, and discuss the mechanisms behind these approaches. Citations
By Monazza Ahmad, B.Pharm, MSc To ensure best health outcomes in a healthcare setting, it is important to establish open, effective, and respectful communication between a patient and a healthcare practitioner. As a patient, it is not only your right but in your best interest to ask your doctor for clarification or further explanation on your health condition and treatment plan. As a healthcare provider, it is your responsibility to provide a safe and comfortable environment for your patients to openly discuss their health concerns and make sure your diagnosis and treatment plan is well understood. That said, menopause can trigger many complex and confusing symptoms that can be uncomfortable to talk about, which can make managing the symptoms difficult. When should I talk to my doctor about menopause?1 First of all, don’t feel awkward. Menopause is a natural phase of life, and your doctor is likely familiar with all possible symptoms. Describe your condition and symptoms in detail and explain how they are affecting your lifestyle and relationships. The provider needs to rule out any other underlying conditions before determining it is menopause. Reach out to your doctor if:
Don’t forget to tell your doctor if you have any allergies or other health conditions. Also mention any medications or supplements you’re already taking for menopause symptoms or other conditions. What shall I ask my doctor? Medical appointments can be stressful, and we often feel rushed. When you have a delicate issue to bring up, being prepared can help. Here are some of the questions you can ask your practitioner:
How can healthcare providers ensure the right care during menopause? Often, the reluctance from healthcare professionals to address these female issues can also cause lack of awareness. It is the healthcare provider’s obligation to make sure patients feel comfortable in discussing their menopausal concerns and understand the treatment plan.2 According to a survey by NIH, patients are likely to discuss menopause transition with providers who don’t make them feel rushed, are good listeners, and have expertise in this area of women’s health. Here are some ways to help your patients receive the best care:
What to ask your patients:3
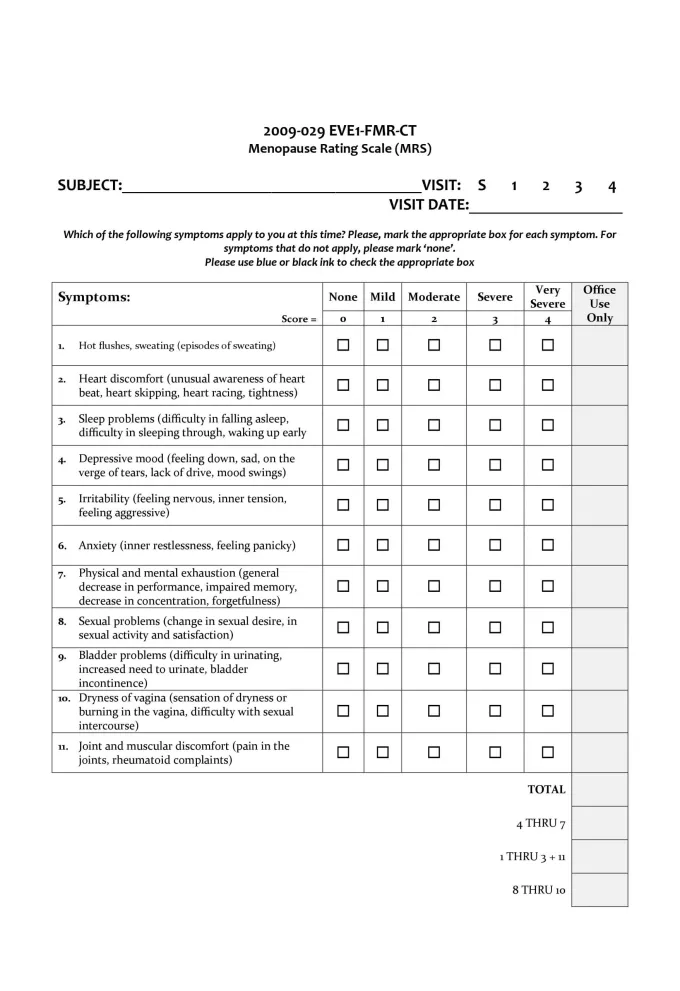
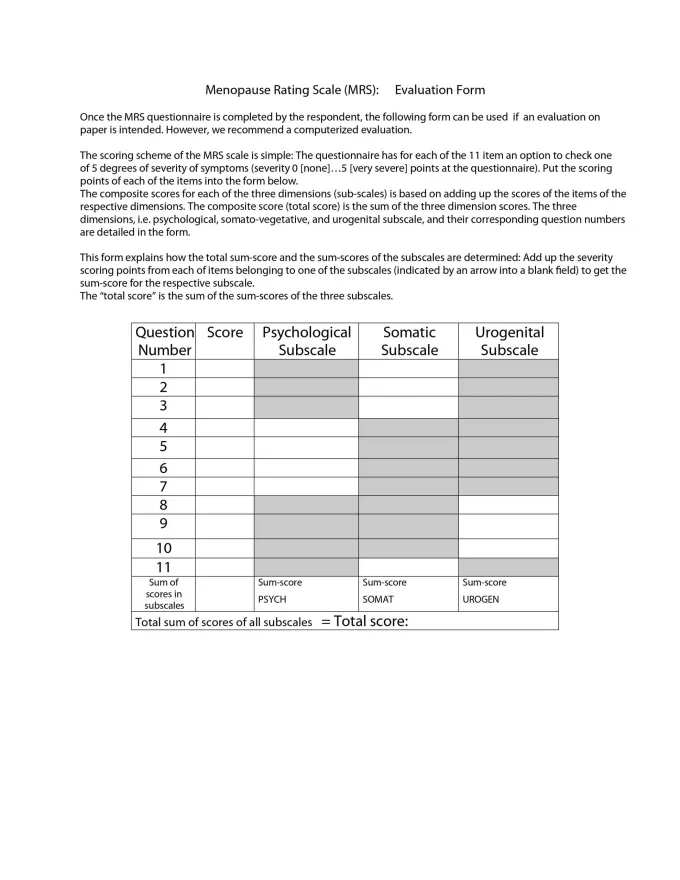
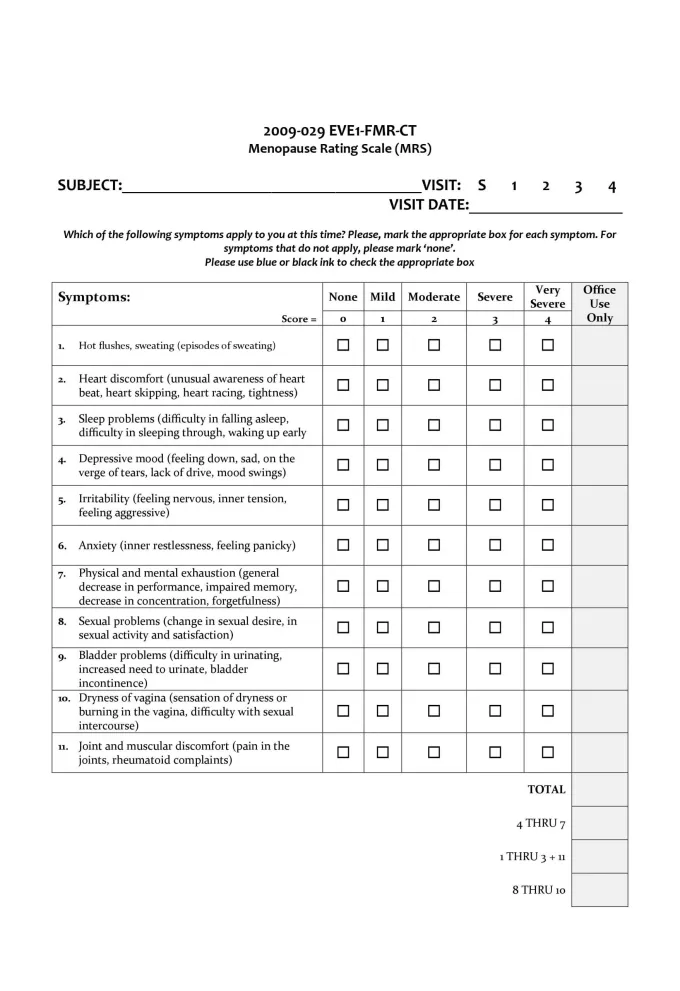
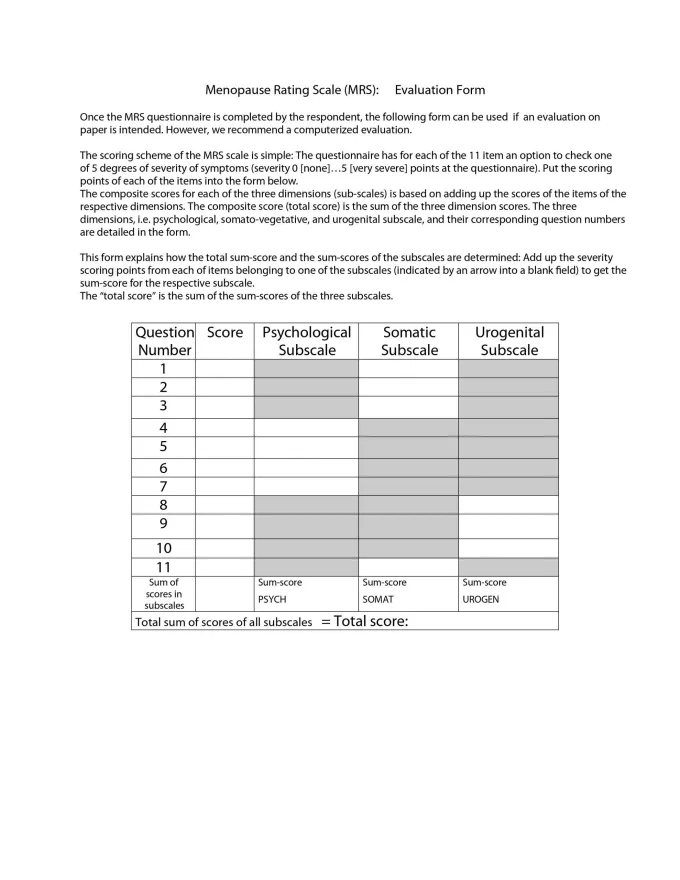
The menopausal rating scale and symptoms evaluation form can be used to track symptom improvement to see what treatment options are working:4,5 Menopause symptoms evaluation form and rating scale (click to enlarge)Menopause is a natural phase in a woman’s life, and its challenges need to be accepted and understood at work, at home, and on a social as well as a societal level. Unless these concerns are progressively communicated in a healthcare setting, it will be tough for us to understand the impact of this condition on a woman’s life.
References:
Feeling bloated during pregnancy? While inconvenient and uncomfortable, most forms of swelling—also known as edema—are perfectly normal for expecting mothers.1
Why does swelling occur during pregnancy? Among the many changes the body goes through during pregnancy is its production and retention of water, blood, plasma, and other fluids to support the needs of the developing fetus.2,3 The swelling supports the mother’s development, as well. Not only does the extra fluid help her body expand to accommodate the baby, it also helps with her body’s necessary changes to prepare for the actual delivery process.1 Most mothers-to-be have swelling in their extremities, as well as in the face.1 Swelling tends to peak during the third trimester, often becoming more noticeable at the end of the day, when extra fluids, blood volume, and the growing baby can affect blood flow in the ankles and feet.4 What other factors affect swelling during pregnancy? A number of factors in addition to the changes taking place in your body can affect swelling.1 These factors include: 1
While mild swelling is acceptable during pregnancy, a very sudden bout of edema could actually be more concerning.1 Contact your doctor immediately if the swelling is uneven and painful, if it comes on suddenly, or if it is accompanied by shortness of breath or chest pain.5 How can you address swelling during pregnancy? There are a number of strategies you can leverage to reduce swelling during pregnancy.1, 5-7 You might make a point of:
Dietary tips to reduce swellingThere are also a number of dietary tips that can help to reduce swelling during pregnancy. These include:
Additional therapies to tryIn addition, pregnant women might try to lessen swelling and related symptoms by engaging in therapies like:
You can either ask your partner to gently massage your feet and legs with the essential oil or soak your feet in a bowl of warm water mixed with essential oil.6
While research offers mixed results on the link between reflexology and swelling, some experts believe the practice can minimize the discomfort associated with swelling.8 Interested in scheduling a reflexology session? Be sure to select a registered specialist who has extensive experience treating pregnant women. Ultimately, there are a number of best practices for reducing swelling during pregnancy.1,5-8 If you still experience swelling after delivering your baby, simply be patient and allow your body time to heal.5 You may still be going through hormonal changes that exacerbate the swelling.5 And of course, feel free to reach out to your healthcare provider at any time if you have questions. References: 1. American Pregnancy Association Staff. Swelling During Pregnancy. https://americanpregnancy.org/pregnancy-health/swelling-during-pregnancy/. American Pregnancy Association. Accessed August 13, 2019. 2. Widen et al. Body composition changes in pregnancy: measurement, predictors and outcomes. Eur J Clin Nutr. 2014;68(6):643-652. 3. Vricella LK. Emerging understanding and measurement of plasma volume expansion in pregnancy. 2017;106(Suppl 6):1620S-1625S. 4. Tanveer F et al. Frequency of lower extremity edema during 3rd trimester of pregnancy. SAJMS. 2015;1:41-43. 5. UnityPoint Health Staff. Things That Make You Swell When You’re Pregnant.https://www.unitypoint.org/livewell/article.aspx?id=e668bf44-c376-459e-b263-41f48810373a. LiveWell with UnityPoint Health. Accessed August 13, 2019. 6. Baby Centre Medical Advisory Board Staff. Swelling (natural remedies).https://www.babycentre.co.uk/a549316/swelling-natural-remedies. BabyCentre UK. Accessed August 13, 2019. 7. Tobah YB. What causes ankle swelling during pregnancy—and what can I do about it?https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/expert-answers/swelling-during-pregnancy/faq-20058467/. Mayo Clinic. Accessed August 13, 2019. 8. Embong NH et al. Revisiting reflexology: Concept, evidence, current practice, and practitioner training. J Tradit Complement Med. 2015;5(4):197–206. Difference between vasomotor and other symptoms of menopause
By Monazza Ahmad, B.Pharm, MSc Menopause is undeniably the most confusing phase of a woman’s life. The irregular menstrual cycle and unpredictable biological changes and emotional state can negatively affect her social, work, and daily life. Seeking help for these symptoms could feel awkward since many times women don’t know how to communicate these concerns and whether it would be empathetically understood or not. At times, the complex medical terms associated with menopause can make it tough to follow the course of treatment plan. Let’s discuss the major signs and symptoms of menopause and the terminologies associated with it that may help you understand your situation as well as convey your concerns to your provider. What are vasomotor symptoms (VMS)? The word “vaso” is originated from the Latin1 meaning vessel, and “motor” relates to movement. So vasomotor symptoms are the movement of blood vessels characterized by their constriction and dilation that causes temporary irregular blood pressure that in turn alters the body temperature, making us feel hot or sweat.2 This temperature alteration results in hot flashes and night sweats that are the most common indication of perimenopause and menopause.3,4 Other chronic and progressive symptoms are characterized by vaginal dryness, painful intercourse, and reduced lubrication. It is seen in both premenopausal and postmenopausal phases.5 Why do I feel like I’m the only one suffering from these symptoms? During menopausal transition, the vasomotor symptoms impact about 80% of the women in the US and differ widely from region to region.6,7 Even though a variety of symptoms is common during menopause, some are not much reported due to their mild and nonspecific nature. Up to 84% of postmenopausal women tend to just deal with the menopausal discomfort rather than seeking medical attention.5,8 How long do these symptoms last? Don’t worry if you have been experiencing vasomotor symptoms for more than a few years. For many women, it can last over a decade or two, with 4-20 hot flashes daily being common during menopause.9 A new long-term study of women from various races and ethnicities suggests that hot flashes and night sweats can take up to 11 years to resolve for some women. Interestingly, the study further discovered that hot flashes lasted longer, for 9-10 years, if started before the menstrual period ended, while their duration was much shorter, with 3.5 years if women had their first hot flash after the periods ended.10 Some menopausal symptoms can get worse with age as opposed to the other menopausal symptoms that improve with time. How do these symptoms impact women’s quality of life? Hot flashes, night sweats, vaginal dryness, low libido, sleeplessness, and menopausal anxiety all add to the decline in quality of life. The sudden outburst of sweat with hot flashes can be daunting when it occurs in a gathering, making women nervous. Vaginal dryness and decreased interest in sexual activities go hand in hand, impacting intimate relationships. All of these stressful changes in daily routine are enough to make any woman anxious.5 Some of the other concerns include brain fog, urinary incontinence, weight gain, hair loss, bone loss, and heart health, to name a few.11 Therefore, women are highly encouraged to not ignore menopausal discomfort and instead have informed discussions with their healthcare providers to find safe solutions for their health needs.12 What are my relief options? There are several options to reduce the impact of these menopausal symptoms and claim your lifestyle back. The solutions include prescription medications, well-studied supplements, lifestyle changes, and nutrition. Since the trial and error of wrong choices can become painful and lengthy during menopause, it is important to discuss the best option with your provider at the right time. Hormone replacement therapy (HRT): This is the most common prescription option for hot flashes, but it is not usually the first choice. The common forms are tablets, gels, skin patches, injections, and vaginal inserts. HRT is generally best-suited for healthy women and those that are in the early phase of menopause. It is not recommended to start HRT after the age of 60. However, there are some side effects associated with HRT, and it is generally considered unsafe for people with a history of heart conditions, deep vein thrombosis, cancer, and smoking.12 Rheum rhaponticum (ERr 731®): This nonhormonal solution is the top recommended natural ingredient by OBGYNs. It has shown to improve 12 of the main menopausal symptoms by 83%. In addition to hot flashes and night sweats, it also improves sleep disturbances, mood swings, sexual discomfort, anxiety, vaginal dryness, and muscle and joint health, to name a few.13 Lifestyle: Daily physical activity is important for menopausal symptom relief. Weight management, stress relief, increased metabolism, and improved overall quality of life as a result of active movement are all related to better management of menopause.14 Eating habits, consuming a healthy diet, practicing relaxation or meditation, drinking enough water, getting quality sleep, and avoiding smoking and alcohol all help with relieving the menopausal discomfort.15 Nutrition: Taking necessary supplements or eating food rich in vitamin D, E, B6, folic acid, and omegas help reduce intensity of menopausal symptoms.16 Now that you have learned more about menopausal symptoms and their treatment options, you may want to discuss these concerns with your healthcare provider. In our next post, we will go over a few tips on how a patient and their healthcare provider can effectively communicate these menopausal challenges with each other to come up with the best treatment plan. References:
By Monazza Ahmad, B.Pharm, MSc To ensure best health outcomes in a healthcare setting, it is important to establish open, effective, and respectful communication between a patient and a healthcare practitioner. As a patient, it is not only your right but in your best interest to ask your doctor for clarification or further explanation on your health condition and treatment plan. As a healthcare provider, it is your responsibility to provide a safe and comfortable environment for your patients to openly discuss their health concerns and make sure your diagnosis and treatment plan is well understood. That said, menopause can trigger many complex and confusing symptoms that can be uncomfortable to talk about, which can make managing the symptoms difficult. Here are some tips for both patients and practitioners to start the conversation around menopause and its symptoms that we discussed in our previous post, Menopausal Symptoms. When should I talk to my doctor about menopause?1 First of all, don’t feel awkward. Menopause is a natural phase of life, and your doctor is likely familiar with all possible symptoms. Describe your condition and symptoms in detail and explain how they are affecting your lifestyle and relationships. The provider needs to rule out any other underlying conditions before determining it is menopause. Reach out to your doctor if:
Don’t forget to tell your doctor if you have any allergies or other health conditions. Also mention any medications or supplements you’re already taking for menopause symptoms or other conditions. What shall I ask my doctor? Medical appointments can be stressful, and we often feel rushed. When you have a delicate issue to bring up, being prepared can help. Here are some of the questions you can ask your practitioner:
How can healthcare providers ensure the right care during menopause? Often, the reluctance from healthcare professionals to address these female issues can also cause lack of awareness. It is the healthcare provider’s obligation to make sure patients feel comfortable in discussing their menopausal concerns and understand the treatment plan.2 According to a survey by NIH, patients are likely to discuss menopause transition with providers who don’t make them feel rushed, are good listeners, and have expertise in this area of women’s health. Here are some ways to help your patients receive the best care:
What to ask your patients:3
Menopause symptoms evaluation form and rating scale (click to enlarge)Menopause is a natural phase in a woman’s life, and its challenges need to be accepted and understood at work, at home, and on a social as well as a societal level. Unless these concerns are progressively communicated in a healthcare setting, it will be tough for us to understand the impact of this condition on a woman’s life.
References:
|
Categories
All
Archives
April 2024
|
|
Join Our Community
|
|
Amipro Disclaimer:
Certain persons, considered experts, may disagree with one or more of the foregoing statements, but the same are deemed, nevertheless, to be based on sound and reliable authority. No such statements shall be construed as a claim or representation as to Metagenics products, that they are offered for the diagnosis, cure, mitigation, treatment or prevention of any disease. |










 RSS Feed
RSS Feed